When you are finished with the reading material, scroll to the bottom of the page to read the directions on how to proceed. Thanks & we hope you enjoy the course!
Sports Injuries
What is an Injury?
An injury is an act that hurts or damages the body. Generally, it refers to damage caused by falls, weapons, hits, accidents, and more. Every year, millions of people injure themselves in the U.S.
How Injuries occur
Injuries can occur at play or work, walking across the street, outdoors or indoors, or driving a car. There are different types of injuries, and all of them range from minor to life-threatening.
Types of Injuries
Some of the common types of injuries are:
- Burns
- Wounds
- Animal Bites
- Fractures
- Dislocations
- Bruises
- Electrical injuries
- Sprains and strains
Sports Injuries
What are Sports Injuries?
Sports injuries refer to the types of injury that occur during exercise, athletic activities or sports. Direct impact, overuse commonly cause these injuries or if the force, greater than the part of the body can withstand structurally is applied. In the United States, about 30 million children and teenagers are those who participate in sports. Out of these 30 million, 3 million participants are of 14 years of age and experience sports injuries annually.
- Classification of Sports Injuries
- Sports injuries are classified into two main types:
- Acute sports injuries
- Chronic sports injuries
- Acute sports injuries
Acute sports injuries occur all of a sudden, like a sprained ankle due to an awkward landing.
Chronic sports injuries
Mainly, the chronic sports injuries commonly occur from the repeated overuse of joints or muscle groups. The poor technique and structural abnormalities can also cause these injuries to develop. It is essential to know if a client has a current sports injury before beginning a session. Sometimes more complicated injuries, such as a bone fracture, may mimic a simple ankle sprain. If a client complains of pain in a particular area from a sports-related injury, a referral to a specialist in that area may be most appropriate for the client to get medically evaluated.
Types of Sports injuries
Some of the common types of sports injuries are as follows:
- Hip flexor strain
- ACL tear
- Concussion
- Groin pull
- Shin splints
- Sciatica
- Hamstring strain
- Tennis or golfer’s elbow
- Shoulder injury
- Patellofemoral syndrome
- Ankle Sprain
- Athlete’s foot
- Bursitis
- Fractures
- Cramping muscles
- Delayed onset muscle soreness
- Frozen shoulder
- Iliopsoas syndrome
- Impingement syndrome
- Iliotibial band syndrome
- Overstraining syndrome
- Overuse syndrome
- Plantar fasciitis
- Soft tissue injuries
- Dehydration
- Nosebleed
- Achilles Tendon Injury
- Turf toe
- Tommy John’s Surgery
- Posterior Cruciate ligament injury
- Skier’s Thumb
- Meniscus Tear injury
Now we will discuss all types of sports injuries one by one along with their introduction, signs and symptoms, diagnostic approaches, treatments and preventive measures.
Shin Splints – Symptoms
Medial Tibial syndrome symptoms: the symptoms for the most common type of shin splint, the medial tibial stress syndrome includes pain in the lower tibia during or at the beginning of a workout. Repetitive and intermittent pain, gradually growing pain, severe pain in the morning which decreases through the day, palpations, swelling, bumps, tenderness, lumps and new bone growth in the shin area. Physical symptoms may also include redness, inflammation and repeated trauma.
Compartment Syndrome:
- Muscle enlargement
- Increased pressure
- Increased pain
- Pain due to movement
- Discomfort with exercising
- Little or No tenderness
Stress fracture symptoms:
- Most symptoms of Medial tibial stress syndrome
- Sharp pain
- Increasing pain during exercising
- Excessive tenderness of muscles
Complications in Treatment and diagnosis of Shin Splints
Since it’s difficult to diagnose the shin splints and the right kind, it can lead to underestimation by the doctor and the patient which can worsen the condition.
In most cases, the complication of severe muscular dysfunction can emerge in situations of shin splints, which are often left unnoticed. Cases of shin splints can also be misunderstood as the tissue fatigue and vice versa. The problem is often generalized as common muscular pain.
Causes of Shin Splints
This particular problem can occur due to many reasons. The most common causes of shin splints include:
- Running on hard surfaces
- Using the wrong sized and fitted footwear
- Sudden exertion and workout without stretching warming up
- The weakness of muscles, bones, hips, and ankles
- Overpronation due to flat feet
- Intense and longer workouts
- The reduced endurance of pressure due to inactivity.
- Stress fracture and lesion on the shin bone
- Over supination due to foot displacement
- Training rigorously without a gradual increase
- Lack of flexibility
Risk Factors of Shin Splints
The most important risk factor associated with shin splints is excessive physical stress due to a variety of reasons. Apart from that, there may be other risks involved, such as tissue overloading, biomechanical problems, history, anatomical and posture issues, and tissue fatigue.
Diagnosis of Shin Splints
The diagnosis for Shin splints is relatively tricky since sometimes injury is extremely severe and difficult to treat. Things can get very complicated, and the condition can become extremely persistent. Nonetheless, the primary diagnosis includes a physical examination where the patient is examined for any apparent symptoms of pain and swelling. The doctor may also carefully determine by moving the shin and knee joint in different positions to see if the movement is limited and painful. Numbness is also considered to be one of the initial indications. Once the physical examination and the medical history evaluation is done, the doctor will see for the scope of diagnostic tests. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound will help the doctor to locate and study the internal structures to see any possible damage.
Treatment for Shin Splints
There are different approaches to the treatment of shin splints. The best way to treat this condition is the natural recovery. It should be assisted by resting your legs more and walking less. After the diagnosis, the natural treatment can be helped in the following ways:
- RICE therapy
- Anti-inflammatory medication
- Using accessories in the shoes or supporting shoes.
RICE therapy is a widespread treatment plan for most of the sports injuries that involve pain and swelling. It is followed in the long run after the first aid response at the time of the injury. Shin splints can include pain and swell apart from other symptoms in almost all cases. These are adequately addressed by using ice on the injured area, compressing it with the help of a bandage, and resting the injured area as much as possible.
The treatment options for shin splints may vary from person to person depending on the type of injury and the severity of each case. In most cases, shin splints can heal naturally. If the problem persists, you may visit a doctor who will carry out a physical examination of the condition. In some cases, the doctor may ask you to walk or run to witness the problem. The first thing that you must ensure is to get enough time to rest as your body needs a break to recover. This involves a whole body rest so that your body can focus on healing the injury instead of spending your energy on other activities.
Using ice on the injured area can also help soothe the pain and reduce the swelling in the case of shin splints. Patients are usually advised to continue to do so for a few days several times during a day for 30 minutes. Once the pain has subsided, they can cease the icing protocol.
Treatment for shin splints may also involve aids and insoles for shoes as it allows to reduce pressure on the injured area and put your legs on the right position. The insoles may be made upon request depending on each case. Otherwise, you can buy the default styles from the market.
Medication is also helpful in case of shin splints as it can alleviate pain and reduce swelling. For shin splints, you should use regular OTCs and NSAIDs that are prescribed by your doctor. Unless it’s necessary, you should avoid taking steroid drugs. Due to the side effects. Naproxen and Aspirins work best for these injuries. It’s also important to understand the specific side effects of these medicines and ways to handle them. Some of them may cause ulcers and bleeding. Therefore, you should use them in moderation, and you must take a prescription from a specialist before making them.
Shin splint injuries can be related to the muscles or the bones. Your treatment will also follow depending upon the type of structures that are injured. In case multiple structures as damaged your treatment may take a compound approach. Careful diagnosis and physical examination will tell the cause.
In case of muscle injuries, a standard approach to treatment is the use of foam rollers. Foam rolls consist of soft foam material that can massage and soothe the injured muscles, including fascia. You should use a foam roller multiple times during the day for 10 minutes at least on the shin and thigh. It can relax the fascia muscle and help loosen it. Apart from foam roll, you can also get a had massage on your shin and thigh area gently. It’s recommended to consult an expert regarding a hand massage since you don’t want to cause any damage to the injured area. It can relax the legs as well as feet, allowing better blood flow. As a result, the movement of your injured area can also be improved. If the problem persists after these treatments, it is best to see a doctor regarding your situation. In the case of bone-related injuries, you may experience stress fractures. The treatment for such bone injuries involves active rest as well as isolation of the injured area. This should be followed by injury friendly exercises that don’t involve using legs too much.
The shoes can use insoles and accessories to the shelf and absorb the shocks of walking and standing. The purpose of treatment is to alleviate the symptoms of inflammation and pain, improving the posture and biomechanical issues, and restoration of the muscles. The rehabilitation therapy can take up to 3 months. Exercising, taping and shin massages are effective ways to treat shin splints. In very severe and rare cases, surgery may be required for the problem of shin splints.
Recovery from Shin Splints
Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. Recovery time varies significantly from patient to patient depending on the severity of the condition, the strength of the injured area and other factors. For effective recovery, you should get back to the normal routine activities slowly and gradually according to your doctor’s advice. Once you start using your muscles and bones again, it will complement the complete healing of the injured parts. If the patient were healthy before the injury, the recovery would usually be faster. However, due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the injury can take from a few weeks to 6 months of time to recover.
Here is what you can do to ensure speedy recovery:
- Rest day and night
- Avoid demanding everyday physical activities
- Gradually start easy activities
- Only use prescribed medication
- Eat healthy as it speeds up the recovery
- Visit your doctor for a checkup of tibia cracks
- Once you are fully recovered from shin splints, you will notice that :
- Both your legs are equally flexible
- Both your legs are equally strong
- You don’t feel pain upon compression
- You can run, walk, and jump painlessly.
Sciatica
What is Sciatica?
Sciatica is a common medical condition that results from sports injuries. The condition is characterized by severe and persistent pain in the back, hip and the leg areas which spreads along the way. The most common causes for this pain is pressure and compression on the sciatic nerve which is a primary part of the spinal nerve root in the lower back. This condition can lead to deterioration of the nerve and degeneration of the intervertebral disc.
Sciatica is a painful condition specifically associated with the sciatic nerve caused due to irritation of the nerve. This nerve is the largest one that is found in the human body, and also extremely important. One of the main physical characteristics of this nerve is the range of its coverage in our body. Sciatic nerve starts from the nerve roots of the spine located near the tailbone, and it’s spread towards the hip and extends down towards the lower part of the legs. This is why the inflammation and pain in the sciatic nerve can cause terrible back pain that spreads all the way down to the legs, thighs and the knee area. The condition can be mild or in many cases extremely severe. The treatment for this condition also depends on the severity of the pain, the symptoms and the causes behind the pain. Therefore, it’s very important to understand and diagnose the right cause of sciatica.
Causes of sciatica
There can be many different causes which lead to sciatica pain. One of the most common causes of sciatica is a hernia of the disc in the lumbar area which can result in a direct pressure and compression of the sciatic nerve. As a result, this pressure can cause irritation and the inflammation in the sciatic nerve and lead to severe pain which the patient may not be able to endure in some cases. The condition in which the pain due to a hernia or abnormality of the intervertebral disc and irritation of the sciatic nerve is experienced is known as radiculopathy. The pressure on the nerve is also referred to as pinching of the nerve.
The pain and irritation of the sciatic nerve can also occur due to a presence of a tumor, proximal muscular displacement, the presence of adjacent bones causing nerve pinching, inflammatory conditions and infectious conditions in the lumbar area of the spine of a nearby location.
The sciatic pain can also result from internal bleeding that occurs due to an injury or some other reasons, accidental injury, and numerous other reasons which may cause pressure on the area. In females, some instances of pregnancy, the consequences of pregnancy can result in a force on the sciatic nerve which causes pinched nerve symptoms. These symptoms can alleviate and completely get eliminated after the delivery of the baby.
Risk factors associated with the Sciatica
The causes and risk factors for developing sciatic pain are numerous. The most common risk factors include secondary and other underlying health conditions that the patient may already be suffering from. This could consist of degenerative arthritis that resides in the same region of the lumbar spine. Other diseases and health conditions of the proximal region also include terms like slipped disc, lumbar disc disease, and trauma. All these conditions can occur as a result of injuries, heavy blows, and accidents that are usually experienced by the people involved in sports and athletics.
Symptoms of Sciatica
There are several symptoms associated with sciatica pain, and different patients may experience a variety of symptoms which may be more or less different from the other patients. In general, the patients suffering from sciatica pain will experience severe pain that originates at the nerve roots in the lower back lumbar area and extends towards the buttocks, hips, shin, thighs, knees and the lower limbs. Apart from pain, other characteristic symptoms may include a tingling sensation, a feeling of heat and pain radiation from the lower back, a burning sensation, numbness of the back area, and a variety of pain, such as hip pain, lumbar pain, leg pain, and buttock pain, depending on the point of the nerve where the pressure and irritation is experienced. Although sciatic nerve has a lot to do with the back and the tailbone area, it is not necessary that every sciatica patient will experience pain in the lower back region indefinitely. As it’s explained that the pain and the location of the pain vary with and depends on the point where the compression of the nerve is experienced, it may not cause pain in the back region at all. This is one reason that sometimes the pain of sciatica can be misunderstood, mistreated and mistaken as some other condition. However, the proper diagnosis and identification of the condition are extremely important to ensure that proper treatment is administered on the patients. As the severity of the pain progresses, it may cause difficulty or complete limitation for the patient to walk or even move around because of severe pain. Moving from a particular position can cause unbearable pain for some patients. In such cases, these symptoms are alleviated by the administration of medication and certain painkillers. For people involved in sports, sciatica can be a big concern, as it can take away a person’s ability to play for quite a while. In severe cases, the patient may experience an inability to bend, move the waist or the back. Resting in a lying position can be a good and effective way for the treatment as lying down can alleviate the pain and keep the patient at ease for the time being.
Diagnosis of Sciatica
For the diagnosis of sciatica, it’s important to learn about the important physical events taking place in the life of the patients, as well as the history of these events and medical conditions. Since the list of causes is so long, it becomes important to evaluate the patient. In case of sports injuries, it remains most probable that the underlying cause of sciatica is the injury and the compression of the sciatic nerve caused by it. However, in some cases, the injury may not be the only reason for the pain caused by sciatic compression, and there may be some other underlying health condition or reason for the sudden onset of the pain.
Characteristic Pain
Although it’s easy to mistake the sciatica pain with some other kind of pain, the sciatic pain can be identified by specific symptoms, including:
- Persistent pain in either the left leg or buttock or the right leg or buttock.
- Sitting for long periods of time typically results in more pain.
- Specific sensations of tingling, burning and/or searing
- Nerve pressure resulting in numbness, weakness, and disability or difficulty in moving the lower limbs
- Piercing and sharp pain disabling a person from standing up and/or walking.
- Pain spreads through the leg except for the foot in most cases.
This is one reason why the diagnosis of sciatica in some cases can be complicated, because it may be mistaken as another issue. The condition can vary among different clients greatly and present itself in different ways.
The primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. The doctor may also carefully examine by moving the back joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the CT scan will help the doctor to locate and study the internal structures to see any possible damage. In certain cases, the diagnostic test may also make use of electromyogram for the determination of possible sciatic condition.
From acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely and the severity of it. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine position, and the movement and flexion of the hip and legs are examined. The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain and tenderness.
Treatment of Sciatica
The treatment for sciatica is based on the diagnosis, the cause of the pain and depends greatly on the severity of the condition. Mostly the patients can rely on the treatments such as medication, muscular relaxant pills, reducing inflammation with the help of medicine, resting, and physical therapy. The condition can get better with time. However, in certain cases, it can persist and intermittent pain can be experienced. In most cases, the condition is improved, and the pain is alleviated without the need for surgery. However, in severe cases, sports people, as well as other people, may require a surgical procedure to alleviate the symptoms of pain. Cortisone injections are also used for the treatment of sciatica pain.
As the condition of sciatica has so much to do with a variety of specialization subjects, people in different medical sectors can assist and help treat the condition. After the evaluation and diagnosis of sciatica, a variety of generalists, specialists and sub specialists can treat the condition. Specialists in the fields of general medicine, internal medicine, gynecology, family medicine, orthopedic specialists, physiatrists and even neurosurgeons can administer a variety of techniques to treat the condition. Other specialties that deal with sciatica pain also include massage therapists, rheumatologists, chiropractors, physical therapists, acupuncturists, and psychologists. The effectiveness of the treatment therefore greatly depends on the reaching out to the right specialists for your kind of sciatica.
Apart from these factors, an important question is what are the treatment options available to sciatic patients and what approach should be taken to ensure effective treatment? Although the conventionally accepted approach to pain treatment such as resting is widely accepted for most conditions, research shows that for sciatica it isn’t the most amazing way to treat the condition. Therefore, the cause of the sciatica pain is detrimental for the choice of the treatment. Effective treatment may include the treatment of the secondary underlying cause or health condition which is causing the sciatica pain or making use of physical therapy. For chronic forms of sciatica which become persistent, treatment options like transcutaneous nerve stimulators can be effective. Apart from that, the exercising, working out and stretching is quite useful to treat the condition of sciatica and help people get back on their feet. Massage therapy can be helpful for relief of this condition, and in some cases, patients/clients may visit a chiropractor or acupuncturist for relief. On top of physical treatment options, medications and painkillers may also provide relief from pain but can have unwanted side effects. These may also include the medicines for inflammation as well as for depression. Certain drugs are also capable of dimming the ability of our brain to feel pain, which can work for patients suffering from severe sciatica pain. Depending on the severity of the condition and the underlying cause of sciatica, surgical treatment or operation may also be required for certain patients who are suffering from persistent and chronic sciatica with severe pain. Applications and training of pain management also play a significant role in the treatment and alleviation of the symptoms.
Recovery from Sciatica
The recovery time of sciatica varies greatly because of its dependency on the factors such as the underlying cause of the persistent sciatica pain, the severity of the condition and the capability of the patient’s body to recover from the condition. In certain conditions, such as the hernia of the disc, the degenerative lumbar spine syndrome, the back sprains and conditions such as shingles can lead to comparatively quicker recovery as these conditions are temporary, reversible and treatable. Sciatica that occurs due to these conditions can be treatment in a matter of days or a couple of weeks. However, in more severe and persistent cases, sciatica can be something extremely stubborn and persistent. Such a condition is referred to as chronic sciatica and may even require surgical procedures for the alleviation of pain.
Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area, the type of causes of sciatica and other factors. For your part in effective recovery, you should avoid the normal routine activities according to your doctor’s advice. Due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the sciatica pain from injury can take from a few weeks to 6 months of time to recover.
Hamstring Muscle Injuries
What is Hamstring Strain?
A hamstring injury is a strain or tear that is characteristic to the areas of tendons, back, thighs, and the larger muscles. It is most commonly observed in people involved in sports and athletes. Depending on the causes the severity can range from mild to extremely severe.
While many different injuries, such as pulled hamstring can be considered as a hamstring muscle injury, there are certain things common in this condition. Hamstring muscle surgery is common in people who are involved in running, sprinting, exertion, walking too much, rigorous training, and sports such as soccer, football, basketball, and other similar sports that need a lot of movement of the legs and excessive exertion. The condition of a pulled hamstring injury or a strain is involved in the pulling and damage of one or more than one muscles located in the thigh area. In most cases, hamstring pulls, and muscular injuries are easily treatable and don’t cause too much trouble. However, in certain cases, the condition can be extremely severe. Nonetheless, there is a lot that can be done to treat the condition, and surgical procedures are very rarely needed to address the most severe cases.
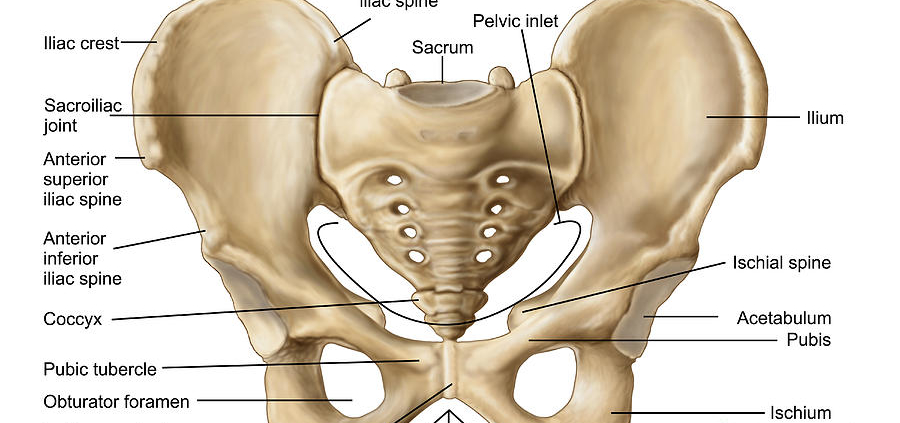
What is a Hamstring Muscle?
Hamstring muscle is a kind of large muscles that extends from the start till the end of the posterior side of thighs. The muscles can be further divided into three main types, namely biceps femoris, semitendinosus, and semimembranosus. These muscles begin from the end of the pelvic region from the point of ischial tuberosity and extend down to intersect the knee joint and crawl further towards the lower part of the leg. These muscles usually consist of strong tissues used for connective purposes, and these are responsible for the power that we have in our legs, which is comparatively a lot more than other parts of our body. These muscles are what helps us with the movement of our leg joints, walking, sitting, bending, lying and everything that our legs are capable of doing.
The injuries and strain related to the hamstring muscles can be in the form of muscle tearing, muscular, complete tearing or the partial tearing of the muscles. The grading of these muscles is dependent on how severe is the damage caused to the muscle. The healing time of hamstring muscle injuries can be as long as three months in case of severe injuries. The most common part that is damaged as a result of hamstring muscle injury is the thicker and core region of the muscles where the tendons and muscles are joined. In the most severe grade 3 cases, the tendons are entirely ripped off from the bones, and in certain cases, a part of the bone is also torn away with it. This most severe type of muscular hamstring injury is referred to as avulsion injury.
Grades of Hamstring Muscle Injuries
There are different grades for Hamstring Muscle Injuries similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three grades are:
- Grade 1: This is the mildest grade for hamstring injuries. It includes less than moderate pain, while the patient retains the ability to feel and move the injured area.
- Grade 2: This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
- Grade 3: This condition usually includes severe pain, while the patient loses the ability to feel and move the injured area.
Causes of Hamstring muscle injuries
There can be a variety of different reasons which can be responsible for mild or severe cases of hamstring muscle injuries. One of the most common cause for Hamstring injury is muscle overload, which can result in the straining of the hamstring muscles. Such a condition may occur if the larger muscle is pulled or stretching too much beyond its threshold of getting back into the place. In this way, it can even get pulled off or ripped off from the bone. This can happen as a result of putting a lot of loads all of a sudden. The most common reasons for this cause include accidents, heavy blows, and sports injuries.
A phenomenon called eccentric contraction can also lead to the occurrence of hamstring muscle strains and injuries due to the lengthening of the hamstring muscles while contracting or shortening. A pressure put on the muscle due to contraction and getting pulled to lengthen it at the same time can result in tearing of the muscle. At the time of running or doing something similar, the eccentric contraction of the muscles is prominently happening. As the running begins, the runner uses the toe to straighten the leg and sprint forward, which is the moment when eccentric contraction takes place. Avulsions are the most severe form of hamstring tendon and muscular injuries, which are caused as a result of putting a lot of load on the tendons all of a sudden.
Risk Factors associated with hamstring muscle injuries
There are some risk factors associated with hamstring muscle injuries. However, the most important ones deserve the attention. The risk of hamstring muscle injury can be increased due to the tightness of muscles which renders it susceptible to strain. Doing light warm-up exercises and stretching before a rigorous sports workout is very important to prevent this type of injury. Another factor is the lack of balance of the muscles due to the difference in the strength of the muscles opposite to each other. Due to such an imbalance, a strain can be caused. Hamstring muscles consist of more powerful front muscles while the posterior muscles are less strong, which can experience fatigue quicker than the stronger muscles on the front. As a result, hamstring muscle injuries and strains can take place. Fatigue can also occur due to other reasons, such as the ability of the muscles to absorb and retain the energy and protect itself from the injuries and heavy blows. Furthermore, another important factor is the condition and the strength of the muscles; if the muscles are strong, they are less likely to get damaged from the exercising, training, pressures and the stress resulting from it. Another factor that matters in determining the risk is the type of activities that a sportsperson chooses to take. Although hamstring muscle injuries can be experienced by any person, certain activities put the people involved in the more at risk of getting a hamstring muscle injury. These activities include certain sports such as basketball, soccer, football, and other activities such as athletics, dancing, running and old age athletics. Since the body is growing unequally at adolescence, people at this age are more at risk of getting a hamstring muscle injury. At the time of growth spurt, bones are capable of growing quicker than the muscles. As a result, the muscles can be pulled and lengthened due to a stretch being caused by a very sudden growth.
Symptoms of Hamstring Muscle injuries
As easy as it is to imagine, hamstring muscle injuries can be very painful at times. The extent of the symptoms however greatly depends on the severity of the injury and the grade. The symptoms that result from hamstring muscles injury includes a sudden and sharp pain in the back region of the thigh due to the injury which will make a sprinting person stop at once or fall terribly. Due to the damage, other symptoms can also show up, such as swelling and redness soon after the injury or after a few hours, bruises and change of color impact on the skin due to internal bleeding or other reasons, and the weakness of the tendons and hamstring muscles which can be prolonged for a couple of months.
Diagnosis for Hamstring Muscle Injury
The primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. The doctor may also carefully examine by moving the thigh and knee joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. An X-ray test will be able to analyze the bone condition. Imaging tests are most important for accurate diagnosis.
By acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely and the severity of it. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine position, and the movement and flexion of the hip and legs are examined.
Treatment for Hamstring Muscle Injuries
Depending on the type and reason of the injury, and the location of the injured area, the treatment for the Hamstring Muscle Injury will be different. The treatment may also be different depending on the consent of the patient as well as the severity and the grade of the injury. The core purpose of the treatment is to normalize the condition of the Hamstring Muscle Injury and achieve painless movement and healing. Only in severe cases, a surgical procedure may be required to treat the Hamstring Muscle Injury. However, in most cases, non-surgical procedures are recommended and opted by the specialists as much as possible. It is very important to comply with the measure and directions of the doctor to ensure effective treatment and restoration of the muscular health.
In most cases of Hamstring injury apart from severe cases, the injuries can easily heal naturally. Nonetheless, you must always make sure that you take enough rest to allow time for your injury to heal. For speeding up the healing and recovery, there are certain measures that you can take.
Icing can be done as an effective way to treat hamstring injuries related symptoms. This involves putting ice on the injured area for up to 15 to 25 minutes several times a day. It should help reduce the swelling and alleviating the pain. Upon the offset of these symptoms, you should stop the icing treatment.
For resting your leg, you need to take some proper measures in hamstring injuries. It can be done bests by avoiding walking, running and all types of sports that involve legs for a while. This will allow your body to focus its energy on healing the injured leg. Resting is more important than other treatments and if you take it for granted other treatments may also not work. Therefore, make sure you don’t put any pressure on the injured leg as it can reverse the healing and cause symptoms to show up again.
Along with resting, you can also consider a physical therapy if you are more concerned about the severity of your condition. A physical therapist will ensure that everything goes smoothly and you can recover quicker. It can also help you avoid stiffness that can be caused due to the lack of activities during the rest period. You should be aiming for the proper stretch, flexibility, and improved movement.
Compression therapy can also be performed as it helps alleviate the symptoms in most cases. Compression is done with the help of a bandage in most cases, but some other technique may be used depending on the type of the injury. This should also be coupled with the elevation technique, the one that you usually see in hospitals. It involves the lifting the leg when the patient is lying down or sitting. At home, you can do this by putting a pillow under your leg as it will allow your leg to elevate. Use multiple pillows if required.
Apart from these physical treatments, you can also opt for medical treatments. In most cases, it won’t be necessary. However, if you’re not able to bear the pain and the acute symptoms, you can opt for medications. The common medicines that are used for hamstring injuries are over the counter drugs, such as Motrin and Advil, or other NSAIDs that can make the pain and other symptoms tolerable. You should understand that these medications work at the cost of side effects. Therefore, if you feel that the pain is better than the side effects that you may suffer from, it is best to avoid taking those medications. Your doctor will carefully examine your condition to tell you if you require medication or not.
Apart from all these treatment options, you can opt for proper exercising. Exercising should not be ignored for the treatment unless otherwise instructed by your doctor or physical therapist. Some of these exercises may be a part of your physical therapy, while there are others that you can try on your own. You must make sure that if any of your exercises in your workout regime is causing even the slightest trouble to your injured area, you must immediately stop doing that and consult your physical therapist to try something else that works for you. Some of the most effective exercises may involve strengthening and stretching exercises. Strengthening exercises should also be a part of your regular workout, as it can prevent you from having a hamstring injury at the first place.
If the problem and symptoms persist and the case is severe, you may require undergoing an operation or a surgery to fix the problem. However, this is very rare, and most hamstring injuries can heal naturally. Surgery may involve the reattachment of a torn hamstring muscle.
Another part of your treatment is to take proper measures to prevent further injury or worsening of the situation. This complementary approach involves the use of aids, crutches and other things that would help to prevent you from getting into further trouble. You should also avoid lifting any weights or putting any pressure on the legs. All of these approaches may be administered until the patient is recovered and the symptoms are gone. You should be able to get back on the sports ground and easily use and move your legs to the full range.
Recovery for Hamstring Muscle Injuries
In most cases, a rehab therapy results in complete recovery from hamstring muscle injuries. Physical therapies along with the RICE treatment can effectively treat the condition and get the patient back on the ground. However, there is a chance of healing process getting reversed if proper measures are not taken and if healing has not completed. Therefore, it’s essential to let your injured muscles recover completely by following the protocol provided by the doctor to eliminate the chances of getting repetitive injuries, chronic conditions, and permanent damage. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area, the type of causes of the Hamstring muscle injury and other factors. For your part in effective recovery, you should avoid the normal routine activities according to your doctor’s advice. Depending on the severity, the Hamstring muscle injury can take from a few weeks to a couple of months of time to recover. Hamstring muscle injuries are painful. Therefore, usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. A regular visit to the doctor will ensure that it’s time to go ahead.
Tennis and Golfer’s Elbow
What Is Tennis and Golfer’s Elbow?
As the name suggests, Tennis and Golfer’s elbow is a condition that usually occurs in people involved in certain types of sports that makes use of the arm extensively. The condition is characterized by inflammation and pain in the muscles and tendons that serve connective purposes on the arm and the elbow. It specifically functions to enjoin the forearm with the elbow. For Golfer’s elbow, the condition is also known as medial epicondylitis in medical terms. The inner area of the elbow is affected which causes an extending pain towards the forearm. The condition may be mild or severe, and it may be treated easily or require prolonged caring. The painful condition and inflammation are developed due to the overuse and overexertion of the muscles of the arm. This mostly happens in athletes, in cases where the overuse of the arm, too much rotating, gripping and flexing of the wrist can result in inflammation. As a tennis or golf player, one requires to twist swing and rotating the forearm and the muscles located there in certain ways to set up for the right shot. As a result, the muscles and tendons can be damaged, degenerated and get torn.
Nonetheless, the name doesn’t imply that these forms of tendinitis conditions are only experienced by tennis players or golf players. In fact, anyone can experience this type of inflammation of tendons. There are people from other sports as well who experience this condition frequently, such as baseball players, basketball players, and bowling players. The tennis elbow tendinitis is characterized as the inflammation of the outside tendons, while the golf elbow tendinitis is characterized by tendinitis of the inner tendons of the elbow. Tennis elbow is also known as lateral epicondylitis, while the golf elbow is medically termed as medial epicondylitis.
Symptoms for Tennis and Golfer’s Elbow
The patients suffering from golf and tennis elbow can experience several symptoms that can indicate the injury and the severity of the injury. While the symptoms may vary from patient to patient, some of the most commonly observed symptoms of tennis and golf elbow syndrome are:
- Burning sensation inside the elbow (golf elbow)
- Burning sensation outside the elbow (Tennis Elbow)
- Pain in the affected area of the injury which can spread towards the wrist through the forearm.
- Numbness of the elbow
- The weakness of the elbow
- Difficulty and pain in the movement of the elbow
- The difficulty, pain, and weakness in the movement of the wrist
- Difficulty in gripping the objects
- Tenderness inside of the elbow and extending along with the tendons
- Swelling of the affected area
- The stiffness of the injured area
- Pain during the gripping and fisting of the wrist.
- Tingling and numbing sensations on the elbow which is extended towards the forearm and the wrist
- Difficulty in doing everyday things, such as pouring coffee, shaking hands, moving the arm, and typing on the keyboard.
Both injuries are usually the result of repetitive strain on the tendons, and although you don’t have to be a golfer or tennis player to experience them, the repeated forceful motions involved in both sports make them very common.
Treatment for Tennis and Golfer’s Elbow
Natural and non-invasive treatments are usually recommended for tennis and golfer’s elbow syndromes. The right approach to treat this condition is the treatment of the causes instead of alleviating the symptoms of the condition. It could include a personal treatment plan, healthy diet plan, changes to the lifestyle and exercising regime. Due to the overuse and overexertion, the painful and inflammatory condition can be specifically treated. Tennis elbow is usually experienced by people involved in the different profession and its most commonly found in the people within the age group of 30 to 50 years old. On the other hand, the golf elbow syndrome which affects the inner tendons of the elbow is experienced by people that practice golf, swimming, painting, tennis, rowing, and baseball. Due to the improper use of the technique, gripping and moving repetitively, and throwing and lifting improperly, golf elbow can result in injury to the inner tendons.
Some things should be taken into account, including the type of the injury, the severity of the injury, and the structures that are damaged due to the injury to determine the right and effective type of the treatment for golf or tennis elbow syndrome. However, for mild to moderate conditions the approach for the treatment remains common in most cases. Some of the common and most effective minimally invasive and non-surgical treatment options available are the ones you should start with.
The best approach you can take for the treatment of golfer’s and tennis elbow injuries is to start off with the right treatment options as soon as possible. Earlier treatment can save you from a lot of trouble in the long run as the symptoms keep developing gradually if proper care is not given. The sooner you start with your treatment, the earlier it will be possible for you to continue your sports practices.
The injury can start off slow but gradually develop into severe conditions. Sometimes mild pain is ignored by the players who become a reason for critical conditions. Therefore, it’s imperative that you take proper rest as soon as the symptoms start to show up. The rest usually involve a break on your sports activities and minimizing the use of your arm and elbow. You should immobilize your arm to allow it to heal your injured structures. Once the pain is gone, and you’re able to move the elbow easily, and to the full range, you can continue with your sports again while administering proper preventive measures to avoid recurrence.
If the pain keeps on troubling your arm despite immobility, you can use ice on the injured elbow and nearby area. It can immediately soothe your pain and reduce the swelling. You should also make sure that you don’t use ice directly on your skin to avoid ice burns. You can wrap the ice into some covering, such as a thin cloth or towel, and use it for 25 minutes after every 2 to 3 hours throughout the day. It may take a few days to eliminate pain and swelling with this treatment.
Some patients may decide to take medicines for the tennis and golfer’s elbow syndrome when the discomfort is interfering with everyday tasks. Ibuprofen and aspirin work well for this purpose. Other OTCs are available on the market, and you should go for non-steroid drugs. These medicines may have a side effect, and they should only be used minimally. If these medicines don’t work, alternative medical treatments may be administered, such as injections of corticosteroids for temporary and short-term relief. They are effective regarding alleviating the symptoms. However, it’s not a permanent solution especially in case of severe conditions that take a lot of time to recover. Medical advancements have also unleashed another innovative method of treatment for this injury, which is known as PRP or platelet-rich plasma technique.
Since the immobility and support are important in this regard, you should go for physical aids and braces to keep the injured arm in place and avoid jerking. It can reduce the pressure and the strain on the muscles that are sensitive due to injury. Counterforce braces may be advised by your doctor or physical therapist.
Stretching and strengthening exercises also play an important role in the treatment of tennis and golfers elbow injuries. These exercises can also prevent you from getting an injury and help you avoid secondary injuries. A specific exercise for this type of injury is administered by the physical therapists, which involves the lengthening of the wrist extensor muscles. This exercise is particularly effective for these injuries. For this injury type, some other physical aids can also be used to support your arm and limiting the movement, such as strapping, braces, supporting pads and other aids that are relevant to arm support. You should also ensure that corrective measures are taken, as the very cause of your tennis or Golfer’s elbow could be wrong training practices and angles of movement. By improving the movement of your arm and elbow joint especially for overhead movements, and by improving your posture you can avoid these injuries as well as speed up the treatment process.
Compressing the elbow region that is injured with a bandage or a wrap can also alleviate the symptoms very effectively. It can also hold the elbow into place and help you reduce unnecessary movement. The treatment involves gradual rehabilitation, which means that you should continue with the treatment measures and gradually return to your sports or other daily activities. You should also inform your trainer or instructor about the condition, and he will make sure that you play the safe way after returning from the treatment.
In severe cases, you should keep a regular contact with your doctor who will closely monitor the condition and the improvement occurring over time. If the condition doesn’t show significant improvement, your doctor may consider certain operation and surgery options for you. The surgery may differ from person to person, and it is rarely administered. However, if no other treatment options are effective, you may immediately need invasive surgery. Usually, the doctor will closely monitor your condition for up to one year and try his best to treat you with non-surgical treatment options. However, in certain cases, the damage is not recoverable naturally, and a surgical aid may be required. The latest surgical procedures involve the removal of damaged tendons from the injured area.
A relatively different approach to the treatment of pain and inflammatory conditions developed by tennis or golfer’s syndrome is the acupuncture technique. It is scientifically accepted by many specialists and can be quite effective for alleviation of the pain. This can be coupled with massaging as well. Both of these traditional treatments can be useful for some patients. Some other less common treatment options include cortisone injections, platelet rich plasma technique, and operation or surgery.
Recovery for the tennis and Golfer’s Elbow
Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area and other factors. It can take anywhere from a week to some months. For effective recovery, you should get back to the normal routine activities slowly and gradually according to your doctor’s advice. Once you start using your muscles and bones again, it will complement the complete healing of the injured parts. If the patient were healthy before the injury, the recovery would usually be faster. However, due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the injury can take up to 6 months of time to recover.
Shoulder Injuries
What are Shoulder Injuries?
The shoulder injuries can be a very common type of injuries when it comes to sports. It can be considered as one of the most mobile and easily dislocated joints in the human body. Due to this factor, athletes and people involved in similar activities are very much susceptible to get such a condition. For the sports people and the people involved in athletes, this can be caused due to rigorous movement of the shoulder, overuse of the shoulder joint, too much taxing of the shoulder, overhead movements involved in certain sports, and too many repetitive movements. Many sports utilize the movement of the shoulder joint to ensure the proper shots, such as cricket, baseball, basketball, badminton, golf, tennis, bowling and other similar sports which also makes it prone to injury. If you’re an athlete, taxing your shoulder over time with repetitive, overhead movements or participating in contact sports may put your shoulder at risk for injury.
The shoulder injuries is a broad term, and therefore it can be classified in many different conditions and injuries that are associated with the shoulder. Each condition is characterized by the type of the injury, the type of body parts impacted by the injury, the severity of the injury and the causes of it. Concerning sports, these injuries related to shoulders can be classified into three most common types which are mostly experienced by the athletes and the sports people. Here are three of these most common shoulder injuries that are normally seen in the sports arena.
SLAP tear
The slap tear is a very common condition which is often seen in sports people. Our shoulder joint has a localized socket that ensures the proper fixation of the bones. The shoulder socket is covered with a ring of cartilage that is called a labrum. In this condition, the labrum wears and tears due to a heavy blow, jerk, overhead shots, repetition of the movement and the wrong movement of the shoulder. The condition causes acute and severe pain. However, the condition is developed over time with a gradual deteriorating of the cartilage. Which is why it’s very important that if the patient experience even a little pain and discomfort of the shoulder, the condition should not be ignored and proper measures should be taken to ensure that the problem gets resolved. If the condition is not addressed promptly, it can grow and cause more trouble to the patient and even result in permanent damage. Due to this tear, the patient can experience a sudden onset of pain and disability of the proper function of the joint.
Due to this injury, the people involved in sports and the athletics can experience deterioration of their performance and difficulty in moving the shoulder joint the way they are trying to do. The pain can be severe or less severe. However, the patient may feel that something is not wrong with the shoulder and it will pop out and dislocate at any minute with any movement. It is important to know and ensure that the warning signs are observed and not left unnoticed since it can result in a more terrible condition. Some of the most important warning signs include pain and discomfort due to certain movements of the shoulder on certain angles. The movement of the shoulder joint is also reduced in range, and the patient may not be able to mobilize the arm to the full range. It can be mistaken for stiffness and difficulty in stretching. The pain is also characteristic in a way that it’s difficult for the patient to pinpoint and exactly tell the place and location where the pain is coming from. If these symptoms are rightly understood, and proper action is taken at the right time, it can prevent the patient from getting further damage.
Symptoms of SLAP Tear in shoulder injuries
Some of the most common symptoms experienced by the players and sports people suffering from a shoulder injury of SLAP Tear includes:
- Grinding feeling with the movement of shoulder joint
- Prominent sound and friction occurring due to joint shoulder movement
- A clicking feeling or sound occurring due to movement of the shoulder.
- A feeling and a sound of popping in the shoulder joint upon movement.
Shoulder instability
Three factors can make the shoulder more susceptible to dislocation: repetitive overhead movement, previous dislocation, and genetics. Read Causes and Risk Factors for a Dislocated Shoulder
Another very common type of shoulder injury experienced by people involved in sports is the shoulder instability. The condition can be commonly experienced by the athletes, and it can occur in people involved in contact sports, such as soccer, hockey, and rugby. Other types of sports which include the rigorous movement and repetition of the shoulder movement also have a good portion of players experiencing shoulder instability. It is a condition which is characterized by the injury to the muscles, tendons, and ligaments. As the name suggests, the instability is caused in the shoulder muscles that are supposed to cover and protect the shoulder joint. As a result, the shoulder joint is left unsecured. The humeral head is the bone of the arm located in the upper part, which gets dislocated due to the instability and the bone can dislocate and pop out completely or partially from the shoulder socket.
Due to this dislocation, the patient can experience a very severe and sudden pain. If the bone is partially dislocated, the pain can be sharp and shocking in the form of bursts and throbs. Along with the pain comes the disability of a person to use their dislocated arm and severe weakness of the shoulder. Concerning physical changes, the patient can also experience severe swelling, discoloration and the bruising on the injured area.
Rotator cuff injury
Another very common type of shoulder injury is the rotator cuff injury. In the Rotator cuff injury, the patient’s condition is caused due to the repetition of the movement of shoulders, overhead movement, overuse of the should joint and other similar activities. People involved in a variety of sports are vulnerable to this condition. Rotator Cuff injuries may be very painful accompanied by the disability to continue sports for a while. The condition makes it very difficult for the patient to sleep, and they may get up from sleep several times during the night due to the shoulder pain. It’s also difficult to get a comfortable lying position where the shoulder doesn’t pain. The pain can get worse with moving the shoulder joint in certain angles, and it can be extended towards the rest of the arm. It can also make the usual everyday activities a challenge for the patient due to the pain, such as combing the hair.
Rotator cuff injuries are also one of the most commonly seen injuries and require more attention. The rotator cuff can be defined as the collection of different tendons and the muscles that are surrounding the shoulder joint and the socket. This is the place where the upper arm is connected strongly to the socket, and this connection is strengthened by the group of tendons and muscles called the rotator cuff. Injury to this group of muscles can result in a dull pain in the shoulder. And the condition can easily get exacerbated while making the pain worse with time. Therefore, proper care, especially with the right sleeping position, is required to treat the condition promptly and not cause further damage.
Causes of injury
If an injury causes a sudden weakness and disability, you should see a doctor as soon as possible. The most common cause in sports for this injury is a hard hit, heavy blow or contact sports. As a result, the wearing and tearing can take place in the Rotator cuff muscles. If the condition is chronic, it can be called as the rotator cuff disease.
Other causes include:
- Overhead strokes and movements
- Repetitive movement
- Sudden jerking
- Heavy hit
- Hard blows
- Falling on the shoulder
How to Diagnose Rotator Cuff Injuries?
The primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The doctor may also carefully examine by moving the knee joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound will help the doctor to locate and study the internal structures to see any possible damage.
Treatments for injury
Physical therapy is a very effective treatment method for the injuries related to the rotator cuff or the shoulder. The treatment may greatly differ depending on the severity of the condition as well as the type of damage an injury that is caused to the shoulder. The treatment aims to bring back the displaced joint or tendons back to their original place, increase the strength and bearing capacity of softer tendons, and improve the flexibility of the tendons and the muscles to keep the shoulder protected. Shoulder injuries may be chronic or acute, and the treatment also differs depending on the type of the injury. Normally, a single heavy blow, jerk or an injury can result in the rotator cuff injury, or the tendons and muscles may get deteriorated over time by repetitive and smaller injuries. Physical or occupational therapy, a sling or shoulder immobilizer, or surgery are the treatments that come into practice the most. You may also take medication along with the treatment, which includes NSAIDS and other over the counter drugs which can be beneficial regarding reducing symptoms and alleviating the pain. In severe cases, bold measures may be taken, and the patient can be given corticosteroid injections and cortisone injections. The approach is only for temporary and only implied if the symptoms are unbearable for the patient. They may also have serious side effects on the patient which is why it is essential to make a favorable decision while deciding to take them.
Regarding home remedies, there are several things that you can do to treat the problems associated with your shoulder. The most important is resting your arm as much as possible and pausing your sports activities for a while. This should quickly fix any mild sprain or strain, and you may not need to get advanced treatment. However, when the symptoms are enhanced, you should try putting the ice on the area for 20 to 30 minutes at least four times a day. You can use a towel wrap to prevent direct contact of the ice with the skin so you can avoid burning. You can also use aids and slings as it can limit the movement of the shoulder in cases of acute injuries. However, you should make sure that you don’t wear the sling for a very long time to avoid stiffness of the shoulder. This is where the exercising and physical therapy becomes important, as you don’t want to jam your shoulder joint by not using it. It will also be helpful in restoring the full range movement of the arm.
Medication can also help in case of shoulder injuries, and the most common medicines that are used for this purpose are ibuprofen and naproxen. However, these medications can interfere with other underlying conditions in a patient. That is why if you are already taking some medicines previously or if you have a previous health condition you should consult the doctor to see if the medicines can react to each other or if they can affect the treatment of other medicines. You should not even use over the counter drugs against or without the prescription of a doctor or a specialist. Depending on the severity of the condition and the type of the structures damaged, it may take as from a few weeks to a few months for you to recover completely and get back to your everyday activities.
Before going for a surgery, you should consider trying other non-surgical options as well. Some of these treatment options for shoulder injuries include:
- Steroid drugs and injections can be administered to reduce the inflammatory conditions in the tight spaces
- Shockwave therapy can be done for shoulder injuries, also known as extracorporeal shockwave therapy. It is a common treatment that is used by orthopedic specialists for various purposes.
- Depending on your case, you may also be a good candidate for a therapeutic ultrasound treatment. Your doctor will examine to determine if you are a good candidate for this treatment or not.
- Another effective treatment for the shoulder injuries is called a dry needling technique. In this treatment is a common treatment administered by physical therapists for various types of injuries. The procedure is also referred to as myofascial trigger point try needling, in which a dry needle is used to treat the pain and the impaired movement without the use of medicine and anesthesia. It is also considered to be an unproven technique by some practitioners, while others find it effective. It could be a preferable substitute for surgery which is more invasive.
- If nothing works, you may opt for surgery. In severe cases, surgery is more viable as it provides a quick fix to severely damaged or torn structures, and it can also clean up other pieces of bones. The reattachment of torn tendons ensures that it’s healed quicker. It can also fix any unnatural tightness or stretch of muscles due to injury.
For surgery, an arthroscopic technique can be used in which the surgeon inserts an arthroscope which can visualize and repair the damage. This is comparatively less invasive as compared to open surgical procedures. Surgery is also a viable option for athletes and sports people who are more interested in their career and wish to get back to the ground as soon as possible. Surgery may also be avoided for people who are above the age of sixty years. In case of rotator cuff injuries, surgery is avoided unless there is a complete tear or a degree 3 injury. The doctor may also choose to go with a surgical procedure if the injury is not responding to non-surgical treatments even after two months from the time of injury.
You may also require surgery if you were involved in a sports activity that required constant use of the shoulder. Apart from that, certain Codman exercises can prove to be helpful for the treatment of shoulder injuries. These are usually administered under the supervision of a physical therapist. It’s aimed at reducing the symptoms of pain and swelling, and enabling the natural full ranged movement of the should joint. This requires a person to lean towards the injured side and hang the arm freely. The patient should move the arm in circles slowly while it’s hanging. The proper diameter and the speed are regulated by the physical therapist, so it should be done under supervision at least for the first few times. Due to the hanging arm, It is also referred to as a pendulum exercise. Apart from that, a broom can also be used for exercising. This is done by gripping the broom with both hands and slowly moving it along a wide arc back and forth gently and slowly as it can make the softer tissues more flexible and stretch them effectively. Resting the shoulder for several days before returning to normal activity and avoiding any movements that might cause pain can be helpful. Limit overhead work or activities. Most shoulder injuries can be treated at home with a proper caring regime.
Risk factors for Rotator cuff Injuries
Risk of rotator cuff injuries is based on some different factors. As a general rule, the overall resilience and strength of the patient is a very detrimental factor. If the muscles are wrong, the injury is likely to be less severe. Apart from that, the strength of the muscles can also be affected by growing age, especially after the age of forty years. Therefore, age is another important risk factor. The type of sports that a person is involved in is also detrimental to the risk. Sports like tennis, baseball, soccer, and golf are the high-risk sports. The professional practices, as well as the medical history of the patient and his family, is also very detrimental.
Complications of Rotator Cuff Injuries
The timely treatment is one of the most important factors when it comes to rotator cuff injuries. If the problem is not addressed promptly and with intensive care, the condition can gradually become worse and even result in permanent damage. It is therefore important to demobilize the shoulder as much as possible and make use of aids like braces and strappings to reduce the movement. If proper care is practiced, the complications are less likely to happen.
Patellofemoral pain syndrome
What is Patellofemoral Pain Syndrome?
The PFPS is one of the very common conditions that are experienced by the people involved in heavy sports, abbreviated as Patellofemoral pain syndrome. In common language, the condition is also called the runner’s knee. The Patellofemoral pain syndrome can be defined as a condition in which the patient experiences the pain in the knee which can either be very severe or less severe. Sometimes it may just be discomfort. However, it should be addressed in the standard way. The back of the kneecap is known as the patella which is connected with the thigh bone, medically known as the femur. The pain is characteristic to the meeting point of the femur and the patella. The condition is different from the other conditions of the knee because of its particular symptom of pain in the anterior knee which involves the retinaculum and the patella. It is difficult to know exactly what the injury is Patellofemoral pain syndrome at the time of the injury, and it may be required to run diagnostics to identify the condition. As the name suggests, the condition is very much common in people who are involved in rigorous and heavy running sports activities and other similar activities. the sports people who experience
Causes of Patellofemoral pain syndrome
Patellofemoral pain syndrome the most are cycling, running, athletics, football, soccer, and hockey. The most common reason is the sudden change in the training practices and the exercise regime of the players, or accidental injuries caused during the running. Another most common cause of Patellofemoral pain syndrome is an accidental injury. Other causes include severe hit, falling on the knee directly, stopping too quickly during a run, and quickly moving in different directions. Women are found to be more prone to patellofemoral pain syndrome in about 62% of cases due to hormonal, anatomical, neuromuscular, and knee laxity factors.
If an injury causes a sudden weakness and disability, you should see a doctor as soon as possible. The most common cause in sports for this injury is a hard hit, heavy blow or contact sports. As a result, the wearing and tearing can take place in the femur and patella. There are several other causes and risk factors associated with the condition of Patellofemoral pain syndrome. The injury can be a result of the wrong kind and size of the shoes which may put pressure on the muscles up along the legs. Other factors are also important such as the intensity of the hit. Overtraining and intense training all also among the most common causes of this condition.
Other causes include:
- Running several steps
- Suddenly stopping while running
- Legs stretching
- Leg displacement or foot displacement while running.
- Wrong posture and legs movement
- Sudden jerking
- Heavy hit
- Hard blows
- Falling on the knee
Signs and symptoms of Patellofemoral Pain Syndrome
The onset of the condition can be gradual over time, or it can be acute due to a sudden injury. Depending on the severity, the signs and symptoms can vary. In less severe cases the patient may experience a sudden discomfort in the knee during a walk or run. Diffuse peripatellar pain is experienced in this condition around the kneecap. In most cases, it’s difficult for the patient to identify the exact location of the pain. The patient may feel and experience a grinding feeling with the movement of the knee. Prominent sound and friction occurring due to knee joint movement are also experienced. The patient may also feel a clicking feeling or sound occurring due to movement of the knee. A feeling and a sound of popping in the knee joint upon movement may also occur. In such cases, the injury includes a pop sound from the knee along with the loss of control over the knee muscle. In severe cases, the movement of the knee joint is severely limited, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling. The patient can experience discomfort while walking, bending knees and while sitting. The everyday activities such as walking up or down the stairs can also become a challenging task.
Diagnosis for Patellofemoral pain syndrome
As discussed before, the diagnosis for the Patellofemoral pain syndrome is not a very simple task. Therefore, a differential diagnosis is commonly carried out for Patellofemoral pain syndrome. The diagnosis of Patellofemoral pain syndrome is complicated and difficult, which is the reason why it can be easily mistaken as another syndrome, such as, Osgood–Schlatter disease. Prepatellar bursitis, Sinding-Larsen, and Johansson syndrome, plica syndrome and patellar tendinitis. There isn’t any single best method for the diagnosis of the Patellofemoral pain syndrome, as the muscle damaged and the conditions can vary among different patients greatly, and some other diseases, problems, and health conditions can result in a similar kind of a pain in the knee. Therefore, a differential diagnosis is administered to eliminate the possibilities of other conditions.
The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case.
Once the initial examination is performed, and the doubts are reduced, the doctor may follow up with diagnostic procedures. The techniques used in this case are radiographic investigations, ultrasonography, the differential diagnosis, and sonographic evaluations. If necessary, the doctor may also use MRI scans to find out the exact location of the damage.
From acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine or elevated position, and the movement and flexion of the knee and legs are examined.
The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain, tenderness of the femur and patella area. The diagnosis also includes the identification of the grading and category for the condition.
Treatment of Sciatica
The treatment for sciatica is based on the diagnosis, the cause of the pain and depends greatly on the severity of the condition. Mostly the patients can rely on the treatments such as medication, muscular relaxant pills, reducing inflammation with the help of medicine, resting, and physical therapy. The condition can get better with time. However, in certain cases, it can persist, and intermittent pain can be experienced. In most cases, the condition is improved, and the pain is alleviated without the need for surgery. However, in severe cases, sports people, as well as other people, may require a surgical procedure to alleviate the symptoms of pain. Cortisone injections are also used for the treatment of sciatica pain.
As the condition of sciatica has so much to do with a variety of specialization subjects, people in different medical sectors can assist and help treat the condition. After the evaluation and diagnosis of sciatica, a variety of generalists, specialists and subspecialists can treat the condition. Specialists in the fields of general medicine, internal medicine, gynecology, family medicine, orthopedic specialists, physiatrists and even neurosurgeons can administer a variety of techniques to treat the condition. Other specialties that deal with sciatica pain also include massage therapists, rheumatologists, chiropractors, physical therapists, acupuncturists, and psychologists. The effectiveness of the treatment therefore greatly depends on the reaching out to the right specialists for your kind of sciatica.
Apart from these factors, an important question is what are the treatment options available to sciatic patients and what approach should be taken to ensure effective treatment? Although the conventionally accepted approach to pain treatment such as resting is widely accepted for most conditions, research shows that for sciatica it isn’t the most amazing way to treat the condition. Therefore, the cause of the sciatica pain is detrimental for the choice of the treatment. Effective treatment may include the treatment of the secondary underlying cause or health condition which is causing the sciatica pain or making use of physical therapy. For chronic forms of sciatica which become persistent, treatment options like transcutaneous nerve stimulators can be effective. Apart from that, the exercising, working out and stretching is quite useful to treat the condition of sciatica and help people get back on their feet. Other treatment options include chiropractic therapy, massage therapy or acupuncture therapy. On top of physical treatment options, medications and painkillers can also prove to be a promising and effective treatment option. These may also include the medicines for inflammation as well as for depression. Certain medicines are also capable of dimming the ability of our brain to feel pain, which can work for patients suffering from severe sciatica pain. Depending on the severity of the condition and the underlying cause of sciatica, surgical treatment or operation may also be required for certain patients who are suffering from persistent and chronic sciatica with severe pain. Applications and training of pain management also play a significant role in the treatment and alleviation of the symptoms.
Recovery from Sciatica
The recovery time of sciatica varies greatly because of its dependency on the factors such as the underlying cause of the persistent sciatica pain, the severity of the condition and the capability of the patient’s body to recover from the condition. In certain conditions, such as the hernia of the disc, the degenerative lumbar spine syndrome, the back sprains and conditions such as shingles can lead to comparatively quicker recovery as these conditions are temporary, reversible and treatable. Sciatica that occurs due to these conditions can be treatment in a matter of days or a couple of weeks. However, in more severe and persistent cases, sciatica can be something extremely stubborn and persistent. Such a condition is referred to as chronic sciatica and may even require surgical procedures for the alleviation of pain.
Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area, the type of causes of sciatica and other factors. For your part in effective recovery, you should avoid the normal routine activities according to your doctor’s advice. Due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the sciatica pain from injury can take from a few weeks to 6 months of time to recover.
Hamstring Muscle Injuries
What is a Hamstring Strain?
A hamstring injury is a strain or tear that is characteristic to the areas of tendons, back, thighs, and the larger muscles. It is most commonly observed in people involved in sports and athletes. Depending on the causes the severity can range from mild to extremely severe.
While some different injuries, such as pulled hamstring can be considered as a hamstring muscle injury, there are certain things common in this condition. Hamstring muscle surgery is common in people who are involved in running, sprinting, exertion, walking too much, rigorous training, and sports such as soccer, football, basketball, and other similar sports that need a lot of movement of the legs and excessive exertion. The condition of a pulled hamstring injury or a strain is involved in the pulling and damage of one or more than one muscles located in the thigh area. In most cases, hamstring pulls, and muscular injuries are easily treatable and don’t cause too much trouble. However, in certain cases, the condition can be extremely severe. Nonetheless, there is a lot that can be done to treat the condition, and surgical procedures are very rarely needed to address the most severe cases.
What is a Hamstring Muscle?
Hamstring muscle is a kind of large muscles that extends from the start till the end of the posterior side of thighs. The muscles can be further divided into three main types, namely biceps femoris, semitendinosus, and semimembranosus. These muscles begin from the end of the pelvic region from the point of ischial tuberosity and extend down to intersect the knee joint and crawl further towards the lower part of the leg. These muscles usually consist of strong tissues used for connective purposes, and these are responsible for the power that we have in our legs, which is comparatively a lot more than other parts of our body. These muscles are what helps us with the movement of our leg joints, walking, sitting, bending, lying and everything that our legs are capable of doing.
The injuries and strain related to the hamstring muscles can be in the form of muscle tearing, muscular, complete tearing or the partial tearing of the muscles. The grading of these muscles is dependent on how severe is the damage caused to the muscle. The healing time of hamstring muscle injuries can be as long as 3 months in case of severe injuries. The most common part that is damaged as a result of hamstring muscle injury is the thicker and core region of the muscles where the tendons and muscles are joined. In the most severe grade 3 cases, the tendons are entirely ripped off from the bones, and in certain cases, a part of the bone is also torn away with it. This most severe type of muscular hamstring injury is referred to as avulsion injury.
Grades of Hamstring Muscle Injuries
There are different grades for Hamstring Muscle Injuries similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three grades are:
Grade 1: This is the mildest grade for hamstring injuries. It includes less than moderate pain, while the patient retains the ability to feel and move the injured area.
Grade 2: This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
Grade 3: This condition usually includes severe pain, while the patient loses the ability to feel and move the injured area.
Causes of Hamstring muscle injuries
There can be a variety of different reasons which can be responsible for mild or severe cases of hamstring muscle injuries. One of the most common cause for Hamstring injury is muscle overload, which can result in the straining of the hamstring muscles. Such a condition may occur if the larger muscle is pulled or stretching too much beyond its threshold of getting back into the place. In this way, it can even get pulled off or ripped off from the bone. This can happen as a result of putting a lot of loads all of a sudden. The most common reasons for this cause include accidents, heavy blows, and sports injuries.
A phenomenon called eccentric contraction can also lead to the occurrence of hamstring muscle strains and injuries due to the lengthening of the hamstring muscles while contracting or shortening. A pressure put on the muscle due to contraction and getting pulled to lengthen it at the same time can result in tearing of the muscle. At the time of running or doing something similar, the eccentric contraction of the muscles is prominently happening. As the running begins, the runner uses the toe to straighten the leg and sprint forward, which is the moment when eccentric contraction takes place. Avulsions are the most severe form of hamstring tendon and muscular injuries, which are caused as a result of putting a lot of load on the tendons all of a sudden.
Risk Factors associated with hamstring muscle injuries
There are some risk factors associated with hamstring muscle injuries. However, the most important ones deserve the attention. The risk of hamstring muscle injury can be increased due to the tightness of muscles which renders it susceptible to strain. This is the reason which makes the warming up and stretching part before getting involved in rigorous sports and works out so important. Another factor is the lack of balance of the muscles due to the difference in the strength of the muscles opposite to each other. Due to such an imbalance, a strain can be caused. This kind of training is usually caused by hamstring muscle due to its size and the scope of imbalance. Hamstring muscles consist of more powerful front muscles while the posterior muscles are less strong, which can experience fatigue quicker than the stronger muscles on the front. As a result, hamstring muscle injuries and strains can take place. Fatigue can also occur due to other reasons, such as the ability of the muscles to absorb and retain the energy and protect itself from the injuries and heavy blows. Furthermore, another important factor is the condition and the strength of the muscles; if the muscles are strong, they are less likely to get damaged from the exercising, training, pressures and the stress resulting from it. Another factor that matters in determining the risk is the type of activities that a sportsperson chooses to take. Although hamstring muscle injuries can be experienced by any person, certain activities put the people involved in the more at risk of getting a hamstring muscle injury. These activities include certain sports such as basketball, soccer, football, and other activities such as athletics, dancing, running and old age athletics. Since the body is growing unequally at adolescence, people at this age are more at risk of getting a hamstring muscle injury. At the time of growth spurt, bones are capable of growing quicker than the muscles. As a result, the muscles can be pulled and lengthened due to a stretch being caused by a very sudden growth.
Symptoms of Hamstring Muscle injuries
As easy as it is to imagine, hamstring muscle injuries can be very painful at times. The extent of the symptoms however greatly depends on the severity of the injury and the grade. The symptoms that result from hamstring muscles injury includes a sudden and sharp pain in the back region of the thigh due to the injury which will make a sprinting person stop at once or fall terribly. Due to the damage, other symptoms can also show up, such as swelling and redness soon after the injury or after a few hours, bruises and change of color impact on the skin due to internal bleeding or other reasons, and the weakness of the tendons and hamstring muscles which can be prolonged for a couple of months.
Diagnosis for Hamstring Muscle Injury
The primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. The doctor may also carefully examine by moving the thigh and knee joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. An X-ray test will be able to analyze the bone condition. Imaging tests are most important for accurate diagnosis.
By acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely and the severity of it. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine position, and the movement and flexion of the hip and legs are examined.
Treatment for Hamstring Muscle Injuries
Depending on the type and reason of the injury, and the location of the injured area, the treatment for the Hamstring Muscle Injury will be different. The treatment may also be different depending on the consent of the patient as well as the severity and the grade of the injury. The core purpose of the treatment is to normalize the condition of the Hamstring Muscle Injury and achieve painless movement and healing. Only in severe cases, a surgical procedure may be required to treat the Hamstring Muscle Injury. However, in most cases, non-surgical procedures are recommended and opted by the specialists as much as possible. It is very important to comply with the measure and directions of the doctor to ensure effective treatment and restoration of the muscular health.
In most cases of Hamstring injury apart from severe cases, the injuries can easily heal naturally. Nonetheless, you must always make sure that you take enough rest to allow time for your injury to heal. For speeding up the healing and recovery, there are certain measures that you can take.
Icing can be done as an effective way to treat hamstring injuries related symptoms. This involves putting ice on the injured area for up to 15 to 25 minutes several times a day. It should help reduce the swelling and alleviating the pain. Upon the offset of these symptoms, you should stop the icing treatment.
For resting your leg, you need to take some proper measures in hamstring injuries. it can be done bests by avoiding walking, running and all types of sports that involve legs for a while. This will allow your body to focus its energy on healing the injured leg. Resting is more important than other treatments and if you take it for granted other treatments may also not work. Therefore, make sure you don’t put any pressure on the injured leg as it can reverse the healing and cause symptoms to show up again.
Along with resting, you can also consider a physical therapy if you are more concerned about the severity of your condition. A physical therapist will ensure that everything goes smoothly and you can recover quicker. It can also help you avoid stiffness that can be caused due to the lack of activities during the rest period. You should be aiming for a proper stretch, flexibility, and improved movement.
Compression therapy can also be performed as it helps alleviate the symptoms in most cases. Compression is done with the help of a bandage in most cases, but some other technique may be used depending on the type of the injury. The bests way to go about it in consultation with an expert, and it’s even better if you let the expert to the job. Once done you can mimic the same approach if it works out for you. This should also be coupled with the elevation technique, the one that you usually see in hospitals. It involves the lifting of the leg when the patient is lying down or sitting. At home, you can do this by putting a pillow under your leg as it will allow your leg to elevate. Use multiple pillows if required.
Apart from these physical treatments, you can also opt for medical treatments. In most cases, it won’t be necessary. However, if you’re not able to bear the pain and the acute symptoms, you can opt for medications. The common medicines that are used for hamstring injuries are over the counter drugs, such as Motrin and Advil, or other NSAIDs that can make the pain and other symptoms tolerable. You should understand that these medications work at the cost of side effects. Therefore, if you feel that the pain is better than the side effects that you may suffer from, it is best to avoid taking those medications. Your doctor will carefully examine your condition to tell you if you require medication or not.
Apart from all these treatment options, you can opt for proper exercising. Exercising should not be ignored for the treatment unless otherwise instructed by your doctor or physical therapist. Some of these exercises may be a part of your physical therapy, while there are others that you can try on your own. You must make sure that if any of your exercises in your workout regime is causing even the slightest trouble to your injured area, you must immediately stop doing that and consult your physical therapist to try something else that works for you. Some of the most effective exercises may involve strengthening and stretching exercises. Strengthening exercises should also be a part of your regular workout, as it can prevent you from having a hamstring injury at the first place.
If the problem and symptoms persist and the case is severe, you may require undergoing an operation or a surgery to fix the problem. However, this is very rare, and most hamstring injuries can heal naturally. Surgery may involve the reattachment of a torn hamstring muscle.
Another part of your treatment is to take proper measures to prevent further injury or worsening of the situation. this complementary approach involves the use of aids, crutches and other things that would help to prevent you from getting into further trouble. You should also avoid lifting any weights or putting any pressure on the legs. All of these approaches may be administered until the patient is recovered and the symptoms are gone. You should be able to get back on the sports ground and easily use and move your legs to the full range.
Recovery for Hamstring Muscle Injuries
In most cases, a rehab therapy results in complete recovery from hamstring muscle injuries. Physical therapies along with the RICE treatment can effectively treat the condition and get the patient back on the ground. However, there is a chance of healing process getting reversed if proper measures are not taken and if healing has not completed. Therefore, it’s essential to let your injured muscles recover completely by following the protocol provided by the doctor to eliminate the chances of getting repetitive injuries, chronic conditions, and permanent damage. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area, the type of causes of the Hamstring muscle injury and other factors. For your part in effective recovery, you should avoid the normal routine activities according to your doctor’s advice. Depending on the severity, the Hamstring muscle injury can take from a few weeks to a couple of months of time to recover. Hamstring muscle injuries are painful. Therefore, usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. A regular visit to the doctor will ensure that it’s time to go ahead.
Tennis and Golfer’s Elbow
What Is Tennis and Golfer’s Elbow?
As the name suggests, Tennis and Golfer’s elbow is a condition that usually occurs in people involved in certain types of sports that makes use of the arm extensively. The condition is characterized by inflammation and pain in the muscles and tendons that serve connective purposes on the arm and the elbow. It specifically functions to enjoin the forearm with the elbow. For Golfer’s elbow, the condition is also known as medial epicondylitis in medical terms. The inner area of the elbow is affected which causes an extending pain towards the forearm. The condition may be mild or severe, and it may be treated easily or require prolonged caring. The painful condition and inflammation are developed due to the overuse and overexertion of the muscles of the arm. This mostly happens in athletes, in cases where the overuse of the arm, too much rotating, gripping and flexing of the wrist can result in inflammation. As a tennis or golf player, one requires to twist swing and rotating the forearm and the muscles located there in certain ways to set up for the right shot. As a result, the muscles and tendons can be damaged, degenerated and get torn.
Nonetheless, the name doesn’t imply that these forms of tendinitis conditions are only experienced by tennis players or golf players. In fact, anyone can experience this type of inflammation of tendons. There are people from other sports as well who experience this condition frequently, such as baseball players, basketball players, and bowling players. The tennis elbow tendinitis is characterized as the inflammation of the outside tendons, while the golf elbow tendinitis is characterized by tendinitis of the inner tendons of the elbow. Tennis elbow is also known as lateral epicondylitis, while the golf elbow is medically termed as medial epicondylitis.
Symptoms for Tennis and Golfer’s Elbow
The patients suffering from golf and tennis elbow can experience several symptoms that can indicate the injury and the severity of the injury. While the symptoms may vary from patient to patient, some of the most commonly observed symptoms of tennis and golf elbow syndrome are:
- Burning sensation inside the elbow (golf elbow)
- Burning sensation outside the elbow (Tennis Elbow)
- Pain in the affected area of the injury which can spread towards the wrist through the forearm.
- Numbness of the elbow
- The weakness of the elbow
- Difficulty and pain in the movement of the elbow
- The difficulty, pain, and weakness in the movement of the wrist
- Difficulty in gripping the objects
- Tenderness inside of the elbow and extending along with the tendons
- Swelling of the affected area
- The stiffness of the injured area
- Pain during the gripping and fisting of the wrist.
- Tingling and numbing sensations on the elbow which is extended towards the forearm and the wrist
- Difficulty in doing everyday things, such as pouring coffee, shaking hands, moving the arm, and typing on the keyboard.
Both injuries are usually the result of repetitive strain on the tendons, and although you don’t have to be a golfer or tennis player to experience them, the repeated forceful motions involved in both sports make them very common.
Treatment for Tennis and Golfer’s Elbow
Natural and non-invasive treatments are usually recommended for tennis and golfer’s elbow syndromes. The right approach to treat this condition is the treatment of the causes instead of alleviating the symptoms of the condition. It could include a personal treatment plan, healthy diet plan, changes to the lifestyle and exercising regime. Due to the overuse and overexertion, the painful and inflammatory condition can be specifically treated. Tennis elbow is usually experienced by people involved in the different profession and its most commonly found in the people within the age group of 30 to 50 years old. On the other hand, the golf elbow syndrome which affects the inner tendons of the elbow is experienced by people that practice golf, swimming, painting, tennis, rowing, and baseball. Due to the improper use of the technique, gripping and moving repetitively, and throwing and lifting improperly, golf elbow can result in injury to the inner tendons.
There are many things that should be taken into account, including the type of the injury, the severity of the injury, and the structures that are damaged due to the injury to determine the right and effective type of the treatment for golf or tennis elbow syndrome. However, for mild to moderate conditions the approach for the treatment remains common in most cases. Some of the common and most effective minimally invasive and non-surgical treatment options available are the ones you should start with.
The best approach you can take for the treatment of golfer’s and tennis elbow injuries is to start off with the right treatment options as soon as possible. Earlier treatment can save you from a lot of trouble in the long run as the symptoms keep developing gradually if proper care is not given. The sooner you start with your treatment, the earlier it will be possible for you to continue your sports practices.
The injury can start off slow but gradually develop into severe conditions. Sometimes mild pain is ignored by the players who become a reason for critical conditions. Therefore, it’s imperative that you take proper rest as soon as the symptoms start to show up. The rest usually involve a break on your sports activities and minimizing the use of your arm and elbow. You should immobilize your arm to allow it to heal your injured structures. Once the pain is gone, and you’re able to move the elbow easily, and to the full range, you can continue with your sports again while administering proper preventive measures to avoid recurrence.
If the pain keeps on troubling your arm despite immobility, you can use ice on the injured elbow and nearby area. It can immediately soothe your pain and reduce the swelling. You should also make sure that you don’t use ice directly on your skin to avoid ice burns. You can wrap the ice into some covering, such as a thin cloth or towel, and use it for 25 minutes after every 2 to 3 hours throughout the day. It may take a few days to eliminate pain and swelling with this treatment.
You can also take medicines for the tennis and golfer’s elbow syndrome if the pain and discomfort are bothering you. Ibuprofen and aspirin work well for this purpose. Other OTCs are available on the market, and you should go for non-steroid drugs. These medicines may have a side effect, and they should only be used minimally. If these medicines don’t work, alternative medical treatments may be administered, such as injections of corticosteroids for temporary and short-term relief. They are effective regarding alleviating the symptoms. However, it’s not a permanent solution especially in case of severe conditions that take a lot of time to recover. Medical advancements have also unleashed another innovative method of treatment for this injury, which is known as PRP or platelet-rich plasma technique.
Since the immobility and support are important in this regard, you should go for physical aids and braces to keep the injured arm in place and avoid jerking. It can reduce the pressure and the strain on the muscles that are sensitive due to injury. Counterforce braces may be advised by your doctor or physical therapist.
Stretching and strengthening exercises also play an important role in the treatment of tennis and golfers elbow injuries. These exercises can also prevent you from getting an injury and help you avoid secondary injuries. A characteristic exercise for this type of injury is administered by the physical therapists, which involves the lengthening of the wrist extensor muscles. This exercise is particularly effective for these injuries. For this injury type, a number of other physical aids can also be used to support your arm and limiting the movement, such as strapping, braces, supporting pads and other aids that are relevant to arm support. You should also ensure that corrective measures are taken, as the very cause of your tennis or Golfer’s elbow could be wrong training practices and angles of movement. By improving the movement of your arm and elbow joint especially for overhead movements, and by improving your posture you can avoid these injuries as well as speed up the treatment process.
Compressing the elbow region that is injured with a bandage or a wrap can also alleviate the symptoms very effectively. It can also hold the elbow into place and help you reduce unnecessary movement. The treatment involves gradual rehabilitation, which means that you should continue with the treatment measures and gradually return to your sports or other daily activities. you should also inform your trainer or instructor about the condition, and he will make sure that you play the safe way after returning from the treatment.
In severe cases, you should keep a regular contact with your doctor who will closely monitor the condition and the improvement occurring over time. If the condition doesn’t show significant improvement, your doctor may consider certain operation and surgery options for you. The surgery may differ from person to person, and it is rarely administered. However, if no other treatment options are effective, you may immediately need invasive surgery. Usually, the doctor will closely monitor your condition for up to one year and try his best to treat you with non-surgical treatment options. However, in certain cases, the damage is not recoverable naturally, and a surgical aid may be required. The latest surgical procedures involve the removal of damaged tendons from the injured area.
A relatively different approach to the treatment of pain and inflammatory conditions developed by tennis or golfer’s syndrome is the acupuncture technique. It is scientifically accepted by many specialists and can be quite effective for alleviation of the pain. This can be coupled with massaging as well. Both of these traditional treatments can be useful for some patients. Some other less common treatment options include cortisone injections, platelet rich plasma technique, and operation or surgery.
Recovery for the tennis and Golfer’s Elbow
Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area and other factors. It can take anywhere from a week to a number of months. For effective recovery, you should get back to the normal routine activities slowly and gradually according to your doctor’s advice. Once you start using your muscles and bones again, it will complement the complete healing of the injured parts. If the patient was healthy before the injury, the recovery would usually be faster. However, due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the injury can take up to 6 months of time to recover.
Shoulder Injuries
What are Shoulder Injuries?
The shoulder injuries can be a very common type of injuries when it comes to sports. It can be considered as one of the most mobile and easily dislocated joints in the human body. Due to this factor, athletes and people involved in similar activities are very much susceptible to get such a condition. For the sports people and the people involved in athletes, this can be caused due to rigorous movement of the shoulder, overuse of the shoulder joint, too much taxing of the shoulder, overhead movements involved in certain sports, and too many repetitive movements. A number of sports utilize the movement of the shoulder joint to ensure the proper shots, such as cricket, baseball, basketball, badminton, golf, tennis, bowling and other similar sports which also makes it prone to injury. If you’re an athlete, taxing your shoulder over time with repetitive, overhead movements or participating in contact sports may put your shoulder at risk for injury.
The shoulder injuries is a broad term, and therefore it can be classified in a number of different conditions and injuries that are associated with the shoulder. Each condition is characterized by the type of the injury, the type of body parts impacted by the injury, the severity of the injury and the causes of it. In terms of sports, these injuries related to shoulders can be classified into three most common types which are mostly experienced by the athletes and the sports people. Here are three of these most common shoulder injuries that are normally seen in the sports arena.
SLAP tear
The slap tear is a very common condition which is often seen in sports people. Our shoulder joint has a localized socket that ensures the proper fixation of the bones. The shoulder socket is covered with a ring of cartilage that is called a labrum. In this condition, the labrum wears and tears due to a heavy blow, jerk, overhead shots, repetition of the movement and the wrong movement of the shoulder. The condition causes acute and severe pain. However, the condition is developed over time with a gradual deteriorating of the cartilage. Which is why it’s very important that if the patient experience even a little pain and discomfort of the shoulder, the condition should not be ignored and proper measures should be taken to ensure that the problem gets resolved. If the condition is not addressed in a timely manner, it can grow and cause more trouble to the patient and even result in permanent damage. Due to this tear, the patient can experience a sudden onset of pain and disability of the proper function of the joint.
Due to this injury, the people involved in sports and the athletics can experience deterioration of their performance and difficulty in moving the shoulder joint the way they are trying to do. The pain can be severe or less severe. However, the patient may feel that something is not wrong with the shoulder and it will pop out and dislocate at any minute with any movement. It is important to know and ensure that the warning signs are observed and not left unnoticed since it can result in a more terrible condition. Some of the most important warning signs include pain and discomfort due to certain movements of the shoulder on certain angles. The movement of the shoulder joint is also reduced in range, and the patient may not be able to mobilize the arm to the full range. It can be mistaken for stiffness and difficulty in stretching. The pain is also characteristic in a way that it’s difficult for the patient to pinpoint and exactly tell the place and location where the pain is coming from. If these symptoms are rightly understood, and proper action is taken at the right time, it can prevent the patient from getting further damage.
Symptoms of SLAP Tear in shoulder injuries
Some of the most common symptoms experienced by the players and sports people suffering from a shoulder injury of SLAP Tear includes:
- Grinding feeling with the movement of shoulder joint
- Prominent sound and friction occurring due to joint shoulder movement
- A clicking feeling or sound is occurring due to movement of the shoulder.
- A feeling and a sound of popping in the shoulder joint upon movement.
Shoulder instability
Three factors can make the shoulder more susceptible to dislocation: repetitive overhead movement, previous dislocation, and genetics. Read Causes and Risk Factors for a Dislocated Shoulder
Another very common type of shoulder injury experienced by people involved in sports is the shoulder instability. The condition can be commonly experienced by the athletes, and it can occur in people involved in contact sports, such as soccer, hockey, and rugby. Other types of sports which include the rigorous movement and repetition of the shoulder movement also have a good portion of players experiencing shoulder instability. It is a condition which is characterized by the injury to the muscles, tendons, and ligaments. As the name suggests, the instability is caused in the shoulder muscles that are supposed to cover and protect the shoulder joint. As a result, the shoulder joint is left unsecured. The humeral head is the bone of the arm located in the upper part, which gets dislocated due to the instability and the bone can dislocate and pop out completely or partially from the shoulder socket.
Due to this dislocation, the patient can experience a very severe and sudden pain. If the bone is partially dislocated, the pain can be sharp and shocking in the form of bursts and throbs. Along with the pain comes the disability of a person to use their dislocated arm and severe weakness of the shoulder. In terms of physical changes, the patient can also experience severe swelling, discoloration and the bruising on the injured area.
Rotator cuff injury
Another very common type of shoulder injury is the rotator cuff injury. In the Rotator cuff injury, the patient’s condition is caused due to the repetition of the movement of shoulders, overhead movement, overuse of the should joint and other similar activities. People involved in a variety of sports are vulnerable to this condition. Rotator Cuff injuries may be very painful accompanied by the disability to continue sports for a while. The condition makes it very difficult for the patient to sleep, and they may get up from sleep several times during the night due to the shoulder pain. It’s also difficult to get a comfortable lying position where the shoulder doesn’t pain. The pain can get worse with moving the shoulder joint in certain angles, and it can be extended towards the rest of the arm. It can also make the usual everyday activities a challenge for the patient due to the pain, such as combing the hair.
Rotator cuff injuries are also one of the most commonly seen injuries and require more attention. The rotator cuff can be defined as the collection of different tendons and the muscles that are surrounding the shoulder joint and the socket. This is the place where the upper arm is connected strongly to the socket, and this connection is strengthened by the group of tendons and muscles called the rotator cuff. Injury to this group of muscles can result in a dull pain in the shoulder. And the condition can easily get exacerbated while making the pain worse with time. Therefore, proper care, especially with the right sleeping position, is required to treat the condition in a timely manner and not cause further damage.
Causes of injury
If an injury causes a sudden weakness and disability, you should see a doctor as soon as possible. The most common cause in sports for this injury is a hard hit, heavy blow or contact sports. As a result, the wearing and tearing can take place in the Rotator cuff muscles. If the condition is chronic, it can be called as the rotator cuff disease.
Other causes include:
- Overhead strokes and movements
- Repetitive movement
- Sudden jerking
- Heavy hit
- Hard blows
- Falling on the shoulder
How to Diagnose Rotator Cuff Injuries?
The primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The doctor may also carefully examine by moving the knee joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound will help the doctor to locate and study the internal structures to see any possible damage.
Treatments for injury
Physical therapy is a very effective treatment method for the injuries related to the rotator cuff or the shoulder. The treatment may greatly differ depending on the severity of the condition as well as the type of damage an injury that is caused to the shoulder. The treatment aims to bring back the displaced joint or tendons back to their original place, increase the strength and bearing capacity of softer tendons, and improve the flexibility of the tendons and the muscles to keep the shoulder protected. Shoulder injuries may be chronic or acute, and the treatment also differs depending on the type of the injury. Normally, a single heavy blow, jerk or an injury can result in the rotator cuff injury, or the tendons and muscles may get deteriorated over time by repetitive and smaller injuries. Physical or occupational therapy, a sling or shoulder immobilizer, or surgery are the treatments that come into practice the most. You may also take medication along with the treatment, which includes NSAIDS and other over the counter drugs which can be beneficial in terms of reducing symptoms and alleviating the pain. In severe cases, bold measures may be taken, and the patient can is given corticosteroid injections and cortisone injections. Although they would reduce the pain. However, they approach temporary and only implied if the symptoms are unbearable for the patient. they may also have serious side effects on the patient which is why it is important to make a favorable decision while deciding to take them.
In terms of home remedies, there are several things that you can do to treat the problems associated with your shoulder. The most important is resting your arm as much as possible and pausing your sports activities for a while. This should quickly fix any mild sprain or strain, and you may not need to get advanced treatment. However, when the symptoms are enhanced, you should try putting the ice on the area for 20 to 30 minutes at least four times a day. You can use a towel wrap in order to prevent direct contact of the ice with the skin so you can avoid burning. You can also use aids and slings as it can limit the movement of the shoulder in cases of acute injuries. however, you should make sure that you don’t wear the sling for a very long time in order to avoid stiffness of the shoulder. This is where the exercising and physical therapy becomes important, as you don’t want to jam your shoulder joint by not using it. It will also be helpful in restoring the full range movement of the arm.
Medication can also help in case of shoulder injuries, and the most common medicines that are used for this purpose are ibuprofen and naproxen. However, these medications can interfere with other underlying conditions in a patient. That is why if you are already taking some medicines previously or if you have a previous health condition you should consult the doctor to see if the medicines can react to each other or if they can affect the treatment of other medicines. You should not even use over the counter drugs against or without the prescription of a doctor or a specialist. Depending on the severity of the condition and the type of the structures damaged, it may take as from a few weeks to a few months for you to recover completely and get back to your everyday activities.
Before going for a surgery, you should consider trying other non-surgical options as well. Some of these treatment options for shoulder injuries include:
- Steroid drugs and injections can be administered to reduce the inflammatory conditions in the tight spaces
- Shockwave therapy can be done for shoulder injuries, also known as extracorporeal shockwave therapy. It is a common treatment that is used by orthopedic specialists for various purposes.
- Depending on your individual case, you may also be a good candidate for a therapeutic ultrasound treatment. Your doctor will carry out an examination to determine if you are a good candidate for this treatment or not.
- Another effective treatment for the shoulder injuries is called a dry needling technique. In this treatment is a common treatment administered by physical therapists for various types of injuries. the procedure is also referred to as myofascial trigger point try needling, in which a dry needle is used to treat the pain and the impaired movement without the use of medicine and anesthesia. It is also considered to be an unproven technique by some practitioners, while others find it effective. It could be a preferable substitute for surgery which is more invasive.
- If nothing works, you may opt for surgery. In severe cases, surgery is more viable as it provides a quick fix to severely damaged or torn structures, and it can also clean up other pieces of bones. The reattachment of torn tendons ensures that it’s healed quicker. It can also fix any unnatural tightness or stretch of muscles due to injury.
For surgery, the arthroscopic technique can be used in which the surgeon inserts an arthroscope which can visualize and repair the damage. This is comparatively less invasive as compared to open surgical procedures. Surgery is also a viable option for athletes and sports people who are more interested in their career and wish to get back to the ground as soon as possible. Surgery may also be avoided for people who are above the age of sixty years. In case of rotator cuff injuries, surgery is avoided unless there is a complete tear or a degree 3 injury. The doctor may also choose to go with a surgical procedure if the injury is not responding to non-surgical treatments even after 2 months from the time of injury.
You may also require surgery if you were involved in a sports activity that required constant use of the shoulder. Apart from that, there are certain Codman exercises that can prove to be helpful for the treatment of shoulder injuries. these are usually administered under the supervision of a physical therapist. It’s aimed at reducing the symptoms of pain and swelling, and enabling the natural full ranged movement of the should joint. This requires a person to lean towards the injured side and hang the arm freely. The patient should move the arm in circles slowly while it’s hanging. The proper diameter and the speed are regulated by the physical therapist, so it should be done under supervision at least for the first few times. Due to the hanging arm, It is also referred to as a pendulum exercise. Apart from that, a broom can also be used for exercising. This is done by gripping the broom with both hands and slowly moving it along a wide arc back and forth gently and slowly as it can make the softer tissues more flexible and stretch them effectively. Resting the shoulder for several days before returning to normal activity and avoiding any movements that might cause pain can be helpful. Limit overhead work or activities. Most shoulder injuries can be treated at home with a proper caring regime.
Risk factors for Rotator cuff Injuries
Risk of rotator cuff injuries is based on a number of different factors. As a general rule, the overall resilience and strength of the patient is a very detrimental factor. If the muscles are wrong, the injury is likely to be less severe. Apart from that, the strength of the muscles can also be affected by growing age, especially after the age of forty years. Therefore, age is another important risk factor. The type of sports that a person is involved in is also detrimental to the risk. Sports like tennis, baseball, soccer, and golf are the high-risk sports. The occupational practices, as well as the medical history of the patient and his family, is also very detrimental.
Complications of Rotator Cuff Injuries
The timely treatment is one of the most important factors when it comes to rotator cuff injuries. If the problem is not addressed in a timely manner and with intensive care, the condition can gradually become worse and even result in permanent damage. It is therefore important to demobilize the shoulder as much as possible and make use of aids like braces and strappings to reduce the movement. If proper care is practiced, the complications are less likely to happen.
Patellofemoral pain syndrome
What is Patellofemoral Pain Syndrome?
The PFPS is one of the very common conditions that are experienced by the people involved in heavy sports, abbreviated as Patellofemoral pain syndrome. In common language, the condition is also called the runner’s knee. The Patellofemoral pain syndrome can be defined as a condition in which the patient experiences the pain in the knee which can either be very severe or less severe. Sometimes it may just be discomfort. However, it should be addressed in the standard way. The back of the kneecap is known as the patella which is connected with the thigh bone, medically known as the femur. The pain is characteristic to the meeting point of the femur and the patella. The condition is different from the other conditions of the knee because of its exclusive symptom of pain in the anterior knee which involves the retinaculum and the patella. Obviously, it is difficult to know exactly what the injury is Patellofemoral pain syndrome at the time of the injury, and it may be required to run diagnostics to identify the condition. As the name suggests, the condition is very much common in people who are involved in rigorous and heavy running sports activities and other similar activities. the sports people who experience
Causes of Patellofemoral pain syndrome
Patellofemoral pain syndrome the most are cycling, running, athletics, football, soccer, and hockey. The most common reason is the sudden change in the training practices and the exercise regime of the players, or accidental injuries caused during the running. Another most common cause of Patellofemoral pain syndrome is an accidental injury. Other causes include severe hit, falling on the knee directly, stopping too quickly during a run, and quickly moving in different directions. Women as found to be more prone to Patellofemoral pain syndrome injuries due to the tenderness of muscles and tendons, while men may also experience tearing and spraining.
If an injury causes a sudden weakness and disability, you should see a doctor as soon as possible. The most common cause in sports for this injury is a hard hit, heavy blow or contact sports. As a result, the wearing and tearing can take place in the femur and patella. There are several other causes and risk factors associated with the condition of Patellofemoral pain syndrome. The injury can be a result of the wrong kind and size of the shoes which may put pressure on the muscles up along the legs. Other factors are also important such as the intensity of the hit. Overtraining and intense training all also among the most common causes of this condition.
Other causes include:
- Running several steps
- Suddenly stopping while running
- Legs stretching
- Leg displacement or foot displacement while running.
- Wrong posture and legs movement
- Sudden jerking
- Heavy hit
- Hard blows
- Falling on the knee
Signs and symptoms of Patellofemoral Pain Syndrome
The onset of the condition can be gradual over time, or it can be acute due to a sudden injury. Depending on the severity, the signs and symptoms can vary. In less severe cases the patient may experience a sudden discomfort in the knee during a walk or run. Diffuse peripatellar pain is experienced in this condition around the kneecap. In most cases, it’s difficult for the patient to identify the exact location of the pain. The patient may feel and experience a grinding feeling with the movement of the knee. Prominent sound and friction occurring due to knee joint movement are also experienced. The patient may also feel a clicking feeling or sound occurring due to movement of the knee. A feeling and a sound of popping in the knee joint upon movement may also occur. In such cases, the injury includes a pop sound from the knee along with the loss of control over the knee muscle. In severe cases, the movement of the knee joint is severely limited, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling. The patient can experience discomfort while walking, bending knees and while sitting. The everyday activities such as walking up or down the stairs can also become a challenging task.
Diagnosis for Patellofemoral pain syndrome
As discussed before, the diagnosis for the Patellofemoral pain syndrome is not a very simple task. Therefore, a differential diagnosis is commonly carried out for Patellofemoral pain syndrome. The diagnosis of Patellofemoral pain syndrome is complicated and difficult, which is the reason why it can be easily mistaken as another syndrome, such as, Osgood–Schlatter disease. prepatellar bursitis, Sinding-Larsen, and Johansson syndrome, plica syndrome and patellar tendinitis. There isn’t any single best method for the diagnosis of the Patellofemoral pain syndrome, as the muscle damaged and the conditions can vary among different patients greatly, and a number of other diseases, problems, and health conditions can result in a similar kind of a pain in the knee. Therefore, a differential diagnosis is administered to eliminate the possibilities of other conditions.
The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case.
Once the initial examination is performed, and the doubts are reduced, the doctor may follow up with diagnostic procedures. The techniques used in this case are radiographic investigations, ultrasonography, the differential diagnosis, and sonographic evaluations. If necessary, the doctor may also use MRI scans to find out the exact location of the damage.
On the basis of acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine or elevated position, and the movement and flexion of the knee and legs are examined.
The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain, tenderness of the femur and patella area. The diagnosis also includes the identification of the grading and category for the condition.
Categories of Patellofemoral pain syndrome
There are different grades for Patellofemoral pain syndrome similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three grades are:
Grade 1: This is characterized by less than moderate pain, while the patient retains the ability to feel and move the injured area.
Grade 2: This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
Grade 3: This is characterized by severe pain, while the patient loses the ability to feel and move the injured area.
Treatment for the Patellofemoral pain syndrome
The treatment can be administered in different ways, as the type of injury will determine the treatment. after the initial first aid response, a careful physical examination can give a good idea of the condition, and other tests may be administered to choose the desired treatment. The treatment approach is three-fold: eliminating pain and other symptoms, recovering the damage that is caused to the structures and recovering a full ranged natural movement of the leg. It can be treated naturally at home in cases of mild to moderate injuries. Simple measures can be taken to begin the treatment of patellofemoral pain. You should rest your knee as much as possible and avoid all the activities that involve the knee as it can worsen the condition. Exercises and sports should be paused while everyday activities should be limited.
A number of medicines can also be taken for reducing symptoms if needed. Some of the drugs like ibuprofen, acetaminophen and naproxen sodium can be taken along with other over-the-counter pain relievers. Apart from these anti-inflammatory drugs, other medicines can be used, such as the Glycosaminoglycan polysulfate (GAGPS) are also widely used for the inhibition of enzyme production. Apart from drugs, it’s recommended to have therapy for the treatment. a physical therapist will help you with certain exercises that you can practice throughout the rehabilitation process. These may especially include strengthening exercises, as this type of injury may very well be due to the lack of strength. The muscles surrounding the knee are there to support the joint and control the movement of the knee. Tearing of these muscles can cause dislocation and displacement of the joint. The physical therapy will be used to control the alignment or various muscles, especially related to the hip, thigh, leg, calf, and quadriceps. Apart from therapy supporting aids can be used for keeping the joint and the injured area in the right location and avoiding pressure or strain on it. Knee braces and arch supports are commonly used, and they can also help in to alleviate the pain quicker. Another aid is taping procedure that can reduce the pain and improve the mobility of the knee joint. It can also keep the injured area compressed which is an effective technique for the alleviation of the symptoms. Icing the area should be done after the physical therapy and exercises for the best results. to avoid stiffness and loss of movement, you should also incorporate knee friendly exercises in your treatment regime according to your doctor’s advice. Such as swimming and bicycling.
In worst case scenarios the last resort would be surgery. For the runner’s knee syndrome, the most commonly administered surgical procedures include arthroscopy and realignment surgery depending on the type of the injury and the diagnosis of the condition. In the arthroscopic procedure, the doctor will insert an arthroscope in the injured area which has a preinstalled camera and light. It can be used to view the condition inside and treat it effectively in a minimally invasive manner. The surgeon can reach the injured area with his instruments through the arthroscope. In cases of dislocation and displacement, the surgeon would carry out a realignment procedure. This may require open surgery to realign the knee back to its natural position to fix the stretch and pressure that it is causing on the proximal cartilages.
To speed up the recovery, you should keep up with the regular physiotherapy until the symptoms of pain and swelling are gone, and the knee is capable of a full-ranged movement. The patient should focus on rehabilitation therapies and non-surgical procedures, and operation and surgery should be avoided as much as possible, at least for the first six months. Your doctor will make sure of when it is a good time for you to get back to life and continue with everyday activities. at first, you should be doing light exercises and training which require less movement and jerking. Here is a brief for the quick measure that can be taken for the treatment of Patellofemoral pain syndrome:
- Resting as much as possible
- Icing the aching area
- Using compression bandages
- Anti-inflammatory medication
- Exercising, stretching, friendly workouts
- Gradually start physical activities, don’t rush.
- Surgery as a last resort, if no results and symptoms persist after the treatment.
Ankle Sprain
What is an Ankle Sprain?
Ankle Sprain can be defined as the injuries that are caused to the tendons and the muscles of the ankle that results in palpation, pain and other symptoms. The proximal tendons, connective tendons in the ankle that connects the foot to the leg and the injury to the bone can cause pain. Ankle Sprain can be a common sports injury in many different games and athletic activities. The most common activities include soccer, football, ice hockey, running, tennis, rugby, American football, basketball and other similar games. It is the most common injury experienced by soccer players. Due to the strong involvement of such tendons in these games, groin strains can occur accidentally or when no prevention measures are taken. Usually, the damage is caused when the bone is detached from the tendon accidentally. The Ankle Sprain is a result of twisting and turning of the ankle in displacement and unnatural manner. As a result, the tendons can wear, stretch and tear. These ligaments and the tendons that are holding the bones together may cause them to lose when they are torn.
Categories of Ankle Sprains
There are different grades for Ankle Sprains similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three grades are:
Grade 1: This is characterized by less than moderate pain, while the patient retains the ability to feel and move the injured area.
Grade 2: This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
Grade 3: This is characterized by severe pain, while the patient loses the ability to feel and move the injured area.
The grade of your sprain will determine the time of your recovery and the mode of your treatment.
Causes of an ankle sprain
The most common cause of an ankle sprain is the turning and the twisting of the ankle joint due to displacement. As a result, the ankle is pushed out of its normal and natural position, and it can cause muscular and tendon damage. Such unexpected movements are very common in sports that involve a lot of running and the use of legs. These tearing of the muscles can be very painful at times and could be accompanied with other symptoms such as bruising discoloration and the swelling of the area. Although it’s mostly the tendons, ligaments, and muscles that are damaged or injured due to ankle sprains, it can also damage other structures, such as the blood vessels and cartilages. There are several risk factors involved, such as the types of sports, etc. however, it can occur in people of all ages.
Some of the other most common causes for Ankle Sprain includes:
- Walking on uneven or hard surfaces
- Wearing the wrong sized or kind of shoes
- Rigorous sports activities and feet movements
- Twisting of feet and ankle muscles
- Turning suddenly during a play
- A sudden strain due to kicking
- Running and stopping suddenly
- Continuing sports after mild strains and pain.
- Wrong diagnosis of a previously occurring pain.
- Repeated minor injuries
- Overuse syndrome
- Microtraumas
Symptoms of an Ankle Sprain
An ankle sprain can result in a number of different symptoms, and it may vary from person to person depending on the severity of the condition and the type and location of the injury. However, the most common symptoms that indicate that the patient has an ankle sprain are the following:
- Bruising on the skin
- Discoloration of the injured area
- Tenderness of the injured area
- inability to walk
- Mild to severe pain due to muscular damage
- inability to move the ankle
- swelling on foot or around the ankle
- the stiffness of the injured area
However, since the ankle is prone to a number of different sports-related injuries, it is easy for a person to mistake it with some other underlying condition which can cause a lot of trouble in the future for the patient. Therefore, it is strongly recommended that once such symptoms start to show up after an injury, the patients should reach out to their doctors as soon as possible for the examination of the condition.
How is an Ankle sprain diagnosed?
The diagnosis for an ankle sprain is relatively difficult since there are a number of different injuries that the ankle is susceptible to, and sometimes they can be extremely severe and difficult to treat. Things can get very complicated, and the condition can become extremely persistent. Nonetheless, the primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The doctor may also carefully examine by moving the ankle and foot in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound can sometimes help the doctor to locate and study the internal structures to see any possible damage.
How is an Ankle sprain treated?
An ankle sprain is one of the most common injuries in orthopedics as well as sports. Usually, the severity of the injury ranges from mild to moderate. There are different types of treatments for ankle sprains. One of the most suggested methods is the P.R.I.C.E. method, which is an acronym for protecting, rest, ice, compress, elevate. Generally, the more natural the treatment is, the better. Self-care is certainly one of the most important factors when it comes to ankle sprains. The very first response should be immediate first-aid care to alleviate the symptoms of pain and swelling. After the diagnosis, the doctor will assign to you an easy to follow the treatment plan that you can practice at home.
Around 25 thousand people suffer from ankle sprains in the United States alone. Even if you are not involved in athletic activities, you can get an ankle sprain due to a sedentary lifestyle.
Every day, about 25,000 people in the U.S. suffer an ankle sprain. Ankle sprains occur in both athletes and those with sedentary lifestyles, and they can occur during sports or when walking to carry out daily activities.
The approach should start with proper protection of the injured ankle as much as possible. We can quickly forget our condition and continue with our daily activities. However, an ankle sprain can get worse with something as simple as walking. It is essential to take proper measures to ensure that we do not do anything to aggravate the condition. Protection should be followed by maximum rest, as rest is the most favorable phase for any injury. Not putting pressure on the ankle will allow it the time to heal. Therefore, you should avoid using the injured ankle as much as possible to let the healing elements of our body start acting. You can also use ice on the injured ankle to alleviate the pain and reduce symptoms. Make sure you don’t burn yourself as it can leave marks. Doing it for a few days can significantly lower the pain and even eliminate it completely. Bandaging and wrapping your ankle with an elastic bandage is also a very common practice and works a great deal for the quick recovery. It can keep the ankle from moving or twisting in the wrong direction and also put compression on the ankle which will soothe the painful symptoms. You need to make sure that the pressure is not too much or too little. Too much pressure will cause problems while too little pressure will not work effectively. You should also keep your foot elevated when you are sitting or lying down, as it can increase the blood flow and improve circulation. This will be especially effective for healing the ankle sprain condition quicker.
NSAIDs and OTCs can also be useful as a secondary treatment aid. These drugs can reduce the inflammatory conditions and alleviate the pain. They can also be used for reducing the swelling of the area which can limit the range of movement. The reason we are calling this a secondary treatment is that it will not be helpful and effective in terms of treating the damage. These drugs, such as painkillers can only alleviate the symptoms, which can make it easier for you to bear the pain. Cortisone injection is another viable option for severe cases. In most cases, you will not require to go to a doctor for mild injuries, and it may heal naturally in a matter of days. Knowing a few measures will enable you to take care of the problem by yourself without any assistance from an expert. However, if the pain is severe, you should not hesitate to see a doctor as soon as possible. It could be a torn or broken tendon or ligament which requires an emergency response.
Once you are treated initially, you need to avoid stiffness due to lack of exercise. For that purpose, it’s important that you start with some light activities and gradually increase them. Some of these exercises would include walking, gentle stretching and strengthening exercises according to the advice of your specialist. The balance exercises are the most important ones for the treatment of ankle sprains. These exercises are also called proprioception exercises, which includes simple techniques to strengthen our balance. It involves multiple attempts to balance yourself on the sprained ankle for a short period of time to note your ability. If you feel that the activities are causing more pain to the damaged ankle, you must immediately stop doing those things and consult your doctor about it once again. Moving around can also tell about the severity of the condition and whether or not you require surgery. You will also have to follow a rehabilitation plan during the adjustment period after the treatment. this will ensure that the condition is not reversed.
The most important factor for an effective treatment of ankle sprain is not to delay the treatment for later. You should start with the treatment as soon as possible, in fact right after the injury. The faster you react to the issue, easier it will be for you to get rid of the problem. Your approach should also include wearing the right type of shoes and using aids. You should also completely avoid walking on uneven and rough surfaces. Try not to climb the stairs unnecessarily. You should try to depend on the natural treatment and rehabilitation and avoid surgical procedures and operations. Some of the best ways to go about the treatment of ankle sprain are:
- Resting as much as possible
- Icing the painting area
- Using compression bandages
- Anti-inflammatory medication
- Exercising, stretching, friendly workouts
- Physical Therapy
- Gradually start physical activities, don’t rush.
- If the treatment shows no results and symptoms persist, you may need surgery.
You may undergo a surgery depending on your case. Which surgery is right for you is the question that depends on several factors, such as the severity of your condition and the type and location of the injury. The surgery for your ankle sprain can be done in one of the following ways:
Reconstruction surgery: Reconstruction surgery, as the name suggests, will reconstruct the damaged muscles, tendons and ligaments in the injured area. They may also be replaced by other healthy tendons which will help the repairing and speedy recovery.
Arthroscopy: If the bone and the cartilages are also affected (Usually in the most severe cases) then your doctor may be required to do an arthroscopy.
Self-Care treatments
You need to take care of yourself too. Here are the things that you can do:
- Using not so tight elastic bandages for ankle support.
- Make sure that you are wearing a brace to
- Make sure you’re using aids like crutches if you feel the need
- The elevation part of the RICE treatment will help you lot.
- Take your medication regularly
- Again, rest, rest, and rest. Then repeat.
Preventive measures for an ankle sprain
You can lower your risk for future sprains by:
Prevention
Prevention is always better than care. Several preventive measures should be understood and exercised in the fields. The best way to go about it is to practice the corrective measures and precautionary measures during the training until they become your reflexes. The prevention measures can be classified as primary and secondary preventions, and each one of them has its own importance. The risk factors associated with ankle sprains should also be addressed and taken care of, including the patient’s history of ankle sprains, the strength of the muscles and the previous injuries. The patients who have experienced previous injuries are 2 times more susceptible to experience it again upon a heavy blow.
- Completing the rehabilitation therapy for any previous ankle sprains
- Practice core strengthening exercises
- Taping and using a bandage to wrap ankle not too tightly
- Avoid further damage by braces and right shoes.
- Stretching and warm up
- Careful on the uneven and hard surfaces
- Don’t do overexertion and stop when your body tells you to stop.
- Say no to high heels
Recovery for an ankle sprain
Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area and other factors. Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. For effective recovery, you should get back to the normal routine activities slowly and gradually according to your doctor’s advice. Once you start using your muscles and bones again, it will complement the complete healing of the injured parts. If the patient was healthy before the injury, the recovery would usually be faster. However, due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the injury can take from a few weeks to 6 months of time to recover.
Here is what you can do to ensure speedy recovery:
- Rest day and night
- Avoid highly demanding everyday physical activities
- Gradually start easy activities
- Visit your doctor for a checkup regularly
- Only use prescribed medication
- Avoid intoxication to avoid tripping and falling
- Eat healthy as it speeds up the recovery
Athlete’s Foot or (Tinea Pedis)
What is athlete’s foot?
Athlete’s Foot is a painful condition usually experienced by the people involved in sports and athletics. That is how it has begotten its name, while in medical terminology the condition is called as Tenia Pedis, which means the infection of the foot. This is a condition in which the athletes develop an infection of the foot because of the dermatophyte fungus which grows progressively and becomes resistant to end. Obviously, the most apparent reason for such an infection occurring in athletes is their usual routine of wearing socks and shoes for hours straight in a go, sweating in them while playing and using those wears again. As this infectious fungus thrives in the humid environment, an athlete’s foot tends to be the most suitable breeding ground for this fungus.
Another reason for the occurrence and prevalence of this fungus is that it’s quite contagious and the players of the same team or the ones playing on the same ground are usually at risk of getting it from other players they’re playing with. Due to its contagious nature, you can pick it from things that were previously in use of another person before you who had an athlete’s foot fungus. The infection can sometimes get problematic and spread to the hands as well as the nails of the toes.
Although it may sound like a terrible disease, athlete’s foot is common, not very serious and also very much treatable. The patient or the athlete can retain their ability to continue their sports, unlike other injuries. The only problem is that sometimes this characteristic infection gets to be very tricky and difficult to treat and cure. Certain people are also prone to experiencing persistence of this infection, such as the people who have weaker immune system and defense system of their bodies, or the people who are involved in a certain health condition such as diabetes. In such cases, it’s a good idea to not think for a minute before calling your doctor about your condition once you’ve diagnosed that it is athlete’s foot.
Causes of athlete’s foot
Tinea Pedis or Athlete’s foot can be caused due to many reasons. The most common reasons due to which tinea pedis may occur are when the growth of tinea fungus on the feet is made possible. For the growth, all that the fungus needs are an inoculum and a favorable environment. An inoculum is basically a small number of fungus cells that are very less to be visible to the naked eye, and it can be picked from anywhere upon closure and direct contact with the infected object. In this way, an athlete can catch this fungus from an infected person through direct or indirect contact, or by getting in contact with the surfaces where the fungus is already present. As far as the favorable environment is concerned, the foot of an athlete is already a very warm and moist environment which is a perfect situation for the fungus to grow and thrive.
The infection with tinea pedis has a lot to do with the hygiene practices as well as the behavior of the athletes. There are certain things that you should be aware of as the causes of tinea pedis or athlete’s foot and the ways to avoid them:
Other common causes include:
- Sharing the outfits or footwear with other people
- Being barefoot on the public floor or other places
- Being barefoot in the locker rooms, showers, and swimming pools
- Sharing footwear, like towels, socks and even washed laundry.
- Keeping tight shoes on for hours straight
- Keeping your feet moist not allowing them to dry
- Sweating too much and staying inside your shoes
- Having an open wound, open nail or open injury
- Sharing the lockers and the closets with other people
- Using a common bathroom or shower that other athletes also use
- Catching from water at places like swimming pools.
Symptoms of athlete’s foot
There can be a number of symptoms associated with the condition. Although there aren’t many types of athlete’s foot, it still depends on the severity of the condition. The symptoms that are most common and characteristic to athlete’s foot are:
- burning sensation in the area of the foot, heel, sole and the nails
- stinging sensation in the proximity of the heal, foot, sole and nails
- Itching on the front of the feet, on the sole, ankle and nails.
- Blistering and painful eruptions on the feet
- Skin peeling and cracking due to itching and scratching
- Peeling of skin between the toes and the sole
- Drying of the skin on the affected area
- Discoloration of the skin, the death of surface skin cell
- Devitalized skin with thicker nails
- Discoloration of nails with crumbling toenails
- A detachment of the two nails in severe cases.
How is athlete’s foot diagnosed?
Since it’s an infectious disease and not a physical injury, it will require physical examination as well as microscopic examination for the presence of the fungus characteristic to the athlete’s foot disease. The very first phase of the diagnosis involves a thorough physical examination to check and test for the symptoms that are mentioned above. Once the symptoms are checked, and it’s verified that it’s a fungal infestation, then the doctor will proceed to the examination of the fungus cells under the microscope to study its shape and morphology in order to know if it’s really the one for the athlete’s foot or something else. To achieve this, the doctor will scrape off some skin from the infected area and dissolve it in a solution of potassium hydroxide (KOH), which is why this test is also called as a skin lesion potassium hydroxide examination. The purpose of KOH is to destroy the normal human cells from the sample so that only the resistant fungal cells can survive. After that, these cells are inoculated and studied under a microscope to ensure that it’s the same fungus.
Treatment for athlete’s foot
The purpose of the treatment is to kill, eliminate and destroy the fungus completely that is living there. If some of it is left remaining, it can grow back once the environmental conditions for the fungus are favorable. Therefore, it’s important to follow the entire recovery regime until your doctor gives you the go-ahead sign. The condition is a fungal infection, and it can be treated by the use of the over the counter drugs which has antifungal properties. The application depends on the severity and the dose prescribed by your doctor. If the over the counter antifungal medication doesn’t work, the doctor may prescribe you other oral and topical drugs to treat the underlying condition. Some over the counter drugs that you can use are miconazole, clotrimazole, butenafine, terbinafine, and tolnaftate as they all have antifungal properties. Some home treatments can also turn out to be very effective in some cases and show great results.
Apart from over the counter drugs, the doctor may also ask you to take prescription medications, which may include topical antifungal medication, oral medication, oral steroid or antibiotics in case of bacterial infestation. Soaking your feet in the salt water or vinegar water can help alleviate the wet blisters. For some patients in certain and rare cases, complications can also develop, such as allergic reactions may occur with fungus infestation which can cause excessive blistering. Like we discussed before, the infection can reappear if it wasn’t completely eliminated the first time. a secondary infection may also take place in certain cases, such as a bacterial infection on top of the fungal infection, which can make the condition even worse. The bacterial infection can then enter the bloodstream as well as the lymphatic system causing a lymph node infection.
Prevention for athlete’s foot
There are numerous preventive measures that you can take in order to avoid getting an athlete’s foot infection. These measures include your everyday activities, your behavioral habits, and your hygiene practices. To prevent yourself from catching an athlete’s foot fungus infection, there are certain things that you should take care of. Firstly, you must keep up with the hygienic practices. Sometimes you may feel like you’re clean, but you can’t see the little tiny invisible microorganisms that are waiting to infect you. So always use soap to clean and wash your hands, feet and other exposed parts of the body through the day and work your way through the area between the toes and those that are not usually reached. After you’re done, also dry them soon and use a clean cloth or towel if you use any at all. Killing the fungus is another good way to avoid getting infected by a booming growth of fungus. For that, you should go for a hot water wash of your feet (preferably 140 degrees), and you can also have the over the counter drugs and antifungal medications to kill them. Also, disinfect your shoes instead of never washing or cleaning them even once in a lifetime. You can also use antifungal powder for these purposes which you can put on your feet each day. Avoid sharing the footwear, especially the socks at all costs unless absolutely necessary. The fungus can get accumulated in the fiber, live and grow in there to infect you again. You should also consider using the socks that ensure proper aeration. That way you will not create a damp environment on your feet. Go barefoot when you’re home, and wear breathable shoes if you do. Also by wearing two different pairs every alternating day, you can allow your shoes to get dry which will prevent the growth of fungus.
Recovery for Athlete’s Foot
The severity of the Athlete’s foot infections can range from being mild or severe. There are cases in which the infection is easily treated within a week or so, while in other cases it can take as long as months of time. There are a number of factors that determine the recovery time and the phase of each patient.
Bursitis
What Is Bursitis?
Bursitis is a condition that is characterized by pain in the Bursae. Bursa is the small sacs that are filled with fluids, and they act as the cushions to the bones, tendons, ligaments and the muscles in the proximal locations of the joints. The condition can result in inflammation of the bursae that can cause mild to severe pain. The purpose of bursae is to smoothen the movements of the muscles and joints and reduce the friction due to the impact of grating, irritation, and rubbing. Inflamed. The most common places where bursitis can take place are the elbow, shoulder and the hip joint. However, this condition can also be experienced in the knee, big toe of your feet and the heel.
Causes of Bursitis
There are a number of different causes of bursitis. Specific to the people involved in sports activities, Bursitis can be experienced most commonly due to the overuse and repeated use of a certain area. As most sports require repetitive movement of a certain part of the body, the athletes and sportsmen can become vulnerable to such conditions.
Other causes of bursitis may include:
- Sudden jerking
- Running several steps
- Suddenly stopping while running
- Legs or arms stretching
- Wrong posture and legs movement
- Heavy hit
- Hard blows
- The weakness of the tendons
- Lack of flexibility of the tendons and muscles
- Tearing of the muscles
- Overexertion of joints
- Not stretching or warming up before working out
- Arthritis
- Length difference of legs
- Infection in rare cases
- Gout
- Psoriatic arthritis
- Thyroid disorders
- Reactions of medication
- Abnormal placement or displacement of joints and bones
People who are involved in sports activities such as scrubbing, tennis, golf, skiing, throwing and pitching are more prone to bursitis conditions.
Hip Flexor Strain
What is Hip Flexor Strain?
A hip flexor strain is a tear or stretches in one or more of the muscles which are responsible for the flexion of hips. This tearing or stretching leads to pain in the groin or the front of the hip. Tendonitis of the hip flexors also causes hip pain, but it is a different condition. In hip flexor tendonitis, the inflammation or damage of the tendon occurs that attaches muscles to the upper thigh bone.
What is the Hip Flexors?
Flexors are a group of muscle tissues that are responsible for stretching and adding a range of motion to the area. Flexors of the hip connect the upper part of the large leg bone (femur) to the groin, hip and lower back.
Muscles which are responsible for lifting the knees towards the body are collectively known as hip flexors. The primary work of hip flexors is to bring knee towards the chest and to bend at the waist. These hip flexor muscles include
- the psoas major and iliacus muscles. These muscles are also referred to as iliopsoas
- . the rectus femoris, which is part of one’s quadriceps
Figure 1: Showing Hip flexors, i.e., Iliacus, Psoas Major and Rectus Femoris
Overstretching or overuse of these muscles and tendons can easily result in reduced mobility, injury and accompanying pain.
Causes of Hip Flexor Strain
As discussed before, hip flexor strain usually occurs when one of the hip flexors has been injured, pulled very hard, or torn. Most often, the hip flexor injuries occur due to acute trauma or injury, like pulling a muscle when jumping or running. Activities like martial arts, sprinting, kicking and dancing which put hip flexors under the most strain also causes this. Weakness in the surrounding core muscles is another common cause of hip flexor pain. The contribution of hip flexor muscles in stabilizing the pelvis is not alone. Due to the weakness of lower abdominal muscles, the flexors of the hip are forced to bear more than they can handle, and this results in muscle strain. Athletes who put their hip flexors under stress in their training and sports are more prone to hip flexor injury or strain that may lead to a muscle tear. In sports medicine, sometimes injuries of hip flexors have a strong association with hamstring strains. It is because injured or tightened tissues of hip flexors can put additional pressure on the lower leg tissues which are commonly known as hamstrings.
Sign and Symptoms of Hip Flexor strain
Usually, hip flexor wounds are rarely diagnosed in clinical settings. However, the chief symptom of hip flexor strain is the pain at the front of the hip. Other signs and symptoms of this type of injury include:
- An intense and quick pain in the hip right after hard blow receiving
- Upper leg area tenderness, muscle cramping, and clenching
- Bruising or swelling around the thigh or hip area
- Inability to continue sprinting, kicking or jumping.
- Tightness or stiffness after being stationary, for example after sleeping
- Loss of sensation in the front of the groin or tugging feeling
- Severe, continual discomfort in the upper area of the leg
Symptoms usually get worse when a person with a wound of hip flexors traveling upstairs, tries to lift his or her knee up and towards the torso or attempting to kick, jump or run.
Grades of Hip Flexor Strain
Remember, hip flexor strains are not equal. They all vary from grade 1 to grade 3 in severity. These grades depend on pain levels, muscle damage and functionality of the muscles. These grades of injuries also indicate the expected time of recovery and the level of required treatment.
Hip Flexor Strain Grade 1
This grade allows the full functionality to the hip. However, due to the damage of a small number of muscle fibers, mild pain may occur.
Hip Flexor Strain Grade 2
In this grade, moderate loss of functionality occurs. Due to the damage of a significant number of muscle fibers, moderate pain also occurs.
Hip Flexor Strain Grade 3
This grade causes severe pain and significant loss of functionality due to the damage to all the muscle fibers.
Treatment of Hip Flexor Strain
Hip flexor pain and strain can be treated by many methods, starting from self-administered therapies to surgeries of torn hip flexor for severe cases. Following are the few common treatment options for hip flexor strain:
Pain relief and healing
The protocol of RICE is one of the most effective treatment option and widely used for all kinds of inflammatory-based ailments and injuries. Although RICE protocol can provide benefit and encourage healing at all stages, it is most effective when used within the first 72 hours following the injury.
Rest
Putting too much strain on the hip flexor following injury may cause swelling, inflammation and further damage. Therefore resting, by the time, allows the body to heal itself.
Ice
Applying an ice pack for a few minutes can play an essential role in reducing inflammation and pain.
Compression
A compression bandage helps prevent further injury and reduces swelling and pain.
Elevation
Usually, it is advised to raise the injured part of the body above the heart to reduce inflammation and restrict the blood flow. But this can be difficult when it comes to the hip. Therefore it is recommended to position the hip in a way that it is not the lowermost part of the body.
Activity Modification
Engaging too early in usual exercise routine may result in further damage and can cause chronic hip flexor problem. Therefore, exercises that put stress on the hip flexors and cause pain should be avoided.
Swimming is, however, a great option that does not aggravate hip flexor strain. Another fantastic option is a seated exercise that includes seated yoga or chair cardio.
Contrast Therapy
Contrast therapy utilizes the alternating application of ice and heat. It is one of the best technique which quells inflammation and pain, boosts circulation, and increases the flow of oxygen and nutrients towards the damaged tissue.
This technique can be performed at home, and it is considered a low-risk treatment for hip flexor strain. Keep in mind that the contrast therapy should not be done within the first 72 hours following the hip flexor strain.
Dry Needling
Dry needling also knew as intramuscular stimulation, is the technique that physiotherapists usually recommend to those who have hip flexor strain. In this therapy, acupuncture needles or other needles are used to minimize the muscular pain.
Dry needling is thought to be worked by creating “movement” in the muscles, reducing pain and tightness, and increasing circulation. Sometimes, following this treatment, patients may feel some soreness, just like the pain felt after a strenuous exercise.
Massage
Another effective way to treat hip flexor strain is soft tissue massage. It increases the flow of oxygen to the damaged tissues and stretches out the tight muscles. This technique also aids healing by removing waste products from around the muscles. But it is advised to avoid any form of massage within the first few days following injury as it may exacerbate inflammation.
Medication
Anti-inflammatory medications play an essential role in providing benefit to Grade 3 hip flexor strains and pain. Aspirin and ibuprofen are one of the best over the counter anti-inflammatories that can alleviate symptoms. However, clinical consultation with a specialist is a must before taking medicines as these medications may cause gastrointestinal tract bleeding or irritation
Prevention of Hip Flexor Strain
Preventing hip flexor strain is very easy. Following are the few methods which can help in preventing hip flexor strain:
Always Stretch yourself
One of the leading causes of injuries related to activity is when a person forgets to stretch before activities. Daily stretching plays a vital role in reducing stiffness and improving mobility and flexibility and of this ultimately help prevent hip flexor strain.
Be Supportive
It is recommended to support your groin, hips, and legs with braces or taping techniques. These techniques maintain the alignment of the body and reduce the risk of further injury to the hip flexor and relapse.
Workouts
Exercise that involves raised legs, sprinting motions, or kicking all increase the risk of a hip flexor strain. However as mentioned earlier, yoga or swimming are the alternate options.
Give hips a break
It is better to schedule rest days and give hips a break between strenuous workouts with recovery days. Taking adequate time to rest before returning to the activities provide benefit and prevents the additional damage or re-injury.
Recovery Time for Hip Flexor Strain
For a hip flexor strain, recovery time varies significantly from person to person. The critical dependence factors of recovery are lifestyle factors, general fitness and health, and severity of the strain.
In the majority of the cases, hip flexor strain is dealt with minimally invasive treatments. Minor tears usually take two to three weeks in healing, whereas it may take four to eight weeks to treat the more severe injury. The recovery time of severe hip flexor strain is longer too.
It is, therefore, better to respond quickly to hip flexor strain because this increases the chances of speedy recovery. It is advised too to use RICE protocol, following the hip flexor strain symptoms onset as soon as possible and proper consultation with a specialist or physiotherapist.
ACL Tear
What is ACL Tear?
ACL tear or anterior cruciate ligament tear is one of the most common injuries of the knee, commonly experienced by the sportsmen and athletes. The condition can be excruciating, and the patient could need knee surgery to get it back to normal. However, each case differs and it depends on the severity of the condition.
What is Anterior Cruciate ligament?
The knee joint is a meeting point of three important bones, the tibia, patella, and the femur. Due to the natural knee cap placement, the joint usually remains protected. Four ligaments are also attached to the bones and the joint, which are classified as cruciate ligaments and collateral ligaments. The cruciate ligaments are present on the inside and intercept each other. The upper intercepting ligament is termed as anterior while the one below is called the posterior cruciate ligament. The anterior cruciate ligament protects the femur and tibia and keeps them stable.
ACL Tear
ACL tear and a sprain is a result of injuries to the meniscus, knee structure, ligaments and articular cartilage that is present in the area. These injuries can be graded and classified into three main types, depending on the severity of the injury and type of injury. Type 1 includes less severe injuries and stretching, type 2 tear is comparatively severe and causes looseness, while type 3 is the most severe form in which the ligaments tear and split. If the condition is not treated timely, it may cause further complications. It can also develop a risk of osteoarthritis and deterioration of the joints.
Causes of ACL Tear
The most common cause of an ACL tear is an accidental injury. Other reasons include a severe hit, falling on the knee directly, stopping too quickly during a run, and abrupt movement in different directions. Women as found to be more prone to ACL injuries due to the tenderness of muscles and ligaments, while men may also experience tearing and spraining.
Signs and Symptoms of ACL Tear
Depending on the type of ACL tear or sprain, the signs and symptoms can vary. In less severe cases the patient may experience a sudden discomfort in the knee during a walk or run. In most cases, ACL cases include a pop sound from the knee along with the loss of control over the knee muscle. In severe cases, the movement of the knee joint is severely limited, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling.
Diagnostic Tests for ACL Tear
The primary diagnosis includes a physical examination, where the patient is examined for any apparent symptoms of pain and swelling. The doctor may also carefully examine by moving the knee joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound will help the doctor to locate and study the internal structures to see any possible damage.
Treatment for the ACL Tear
The commonly used RICE treatment plan can treat the condition. The very first response should be immediate first-aid care to alleviate the symptoms of pain and swelling. After the diagnosis, the doctor will assign to you an easy to follow the treatment plan that you can practice at home.
The RICE treatment stands for resting, icing, compressing and elevating. Resting is the most crucial part of the healing process, as a wrong pressure and movement can reverse the healing and make the condition worse. The patient should avoid walking around and bearing any weights. Furthermore, icing can help alleviate the symptoms of pain and swelling, while speeding up the healing process at the same time. The knee area should also be compressed by fastening an elastic wrap around it, and the patient should keep the knees elevated with the help of a pillow whenever they’re laid down. It may take several weeks for the patient to recover through a rehabilitation process. Regular physiotherapy can ensure a speedy recovery, and a variety of different aids can be used for protection, such as crutches and braces. The treatment and rehabilitation should be extended until the symptoms of pain and swelling are gone, and the knee is capable of a full-ranged movement. People who tend to remain inactive and minimize the movement can recover from the injury sooner. Therefore, it is recommended that the patient should get involved in injury-friendly exercises and other tasks that don’t require robust movements.
Surgical treatment for ACL Tears
In certain severe cases, surgery may be required to fix the problem. It becomes critical when the patient needs immediate recovery, when the injury persists, or when the injury keeps bending and displacing the knee. The surgery may also be required if multiple ligaments are injured. In the surgical procedure, the damaged ligament is removed and replaced by another tissue known as a graft, which allows it to heal and recover. The graft may be taken from a donor area which is usually another area of the knee. However, rehabilitation is a must after the surgery. The surgery is minimally invasive and reconstructs the damaged ligament.
Surgery is usually prescribed to the ACL patients, as it can effectively recover the patients bringing them back to the normalized knee condition. However, if the patient isn’t involved in heavy activities, such as jumping, running, too much manual work, or sports, the alternative treatment options can be administered.
The surgical treatment is initiated after a delay of around one month. The delay is to monitor the healing speed of the patient and let the swelling and bleeding reduce. This also gives an idea of the persistence of the injury. Physiotherapies are mainly involved in the post-operative rehabilitation therapy. The recovery highly depends on the consistent care and physiotherapeutic treatment, without which the recovery may be delayed or reversed. It’s important to note that the surgical procedure also requires 7 to 9 months of rehabilitation therapy and the sportsmen can return to the playgrounds after a year. The process starts with light exercises and later on the focus is gradually shifted towards enabling the full-range movement of the knee joint. Flexing and bending your muscles too much should be avoided, and the gradual increase in the exercising routine should be practiced. The rehabilitation therapy also uses aids like crutches and braces to improve the protection level and prevent pressure, jerking and stress.
How to prevent ACL Tears and Injuries?
It’s important to stick to proper training and exercising methods to avoid getting an ACL Tear due to a training accident. Sportsmen and athletes should also be mindful of the possibility of a knee injury and should be aware of measures to prevent the knee from severely damaging in case of an accident, Should be aware of measures to prevent the knee from severely damaging in case of an accident. Another effective way of avoiding ACL tears is to strengthen the core muscles by exercising. Some exercises such as hamstring can help increase the strength and endurance of leg muscles. Stronger legs can also help to reduce the pressure on the knee due to falling. Athletes and sportsmen must also practice techniques of jumping, cutting, pivoting, proper knee positioning and landing to prevent injury from sudden falling.
Concussion
What is Concussion?
Concussions can be described as a condition in which the patient experiences temporary unconsciousness, disorientation, confusion and other symptoms as a result of an injury of the head due to heavy blow or violent shock. Concussions can be a result of traumatic brain injury due to violent shaking or hit. Around 0.2 million were hospitalized due to a concussion during the last decade. It is a common sports injury and should be considered as a grave concern. Our skull is the hardest bone of our body, but it houses the very soft tissues of the brain and neurological parts. An injury to the brain can be extremely severe, and in some cases, it can lead to unconsciousness, memory loss, disability, and death. A sudden hit or blow can damage or puncture the blood vessels, resulting in stroke and other severe conditions. Neuropathic conditions can also develop due to brain injury. If our nerves and neurons are damaged, our brain may not function properly and may not be able to transfer and communicate the signals to the rest of our body. This can result in behavioral changes in the patients.
Concussions can also occur in children due to the larger size of their skull compared to the rest of the body. Due to several physiological changes the children go through, they remain to be more susceptible to the risk of concussions.
Types of Concussions
Similar to ACL Tear as discussed before, concussions are also classified into three different types depending on the severity of the condition and the symptoms that are experienced by the patient, such as unconsciousness, disorientation, memory loss, amnesia, and the loss of balance. On a grade from 1 to 3, the cases of concussions are classified as 1 being least s1 to 3, the cases of concussions are classified as one being least severe, and 3 being the most severe. In the least severe case, the patient may experience the mild symptoms for 10 to 12 minutes before getting back to normal. The patient tends to remain conscious. In type 2 concussion, the patient may experience symptoms for more than fifteen minutes. However, the consciousness is retained. In the most severe type of concussion, the patient becomes unconscious. This consciousness may be regained in 5 seconds, or it may get prolonged.
Causes for Traumatic Brain Injury or Concussions
Causes for concussions and brain injury are most commonly the accidental injuries. People involved in sports and athletics are most prone to such injuries. The most common causes for concussions can be classified into four types:
Falling
Tripping and falling can result in a direct blow and heavy hit on the head if the victims directly land on their head. Deaths due to falling are less frequent, but certainly possible.
Road accidents
Road accidents are one of the leading causes of injuries and deaths.
Heavy Blows
Getting struck by a sharp object of hitting oneself against an object on the head can lead to severe head injuries.
Being attacked
Getting hit on the head by an attacker can lead to severe damage to the head and remains to be the most common cause of concussions.
Regarding sports, many games have a higher risk of getting traumatic brain injuries leading to concussions. Some of the most common games and sports include:
- Ice skating
- Soccer
- Cycling
- Gymnastics
- Skiing/Snowboarding
- Football
Signs and symptoms of Concussions
It is difficult to understand concussion every time as the injury could cause other conditions as well. However, if there are physical signs, swelling, bruising, cut, or bleeding from the head after a hit you need to be attentive to that situation. Since the span of concussion symptoms is very small, a concussion might even go unnoticed. Sometimes the symptoms and signs are unnoticeable at the time of the injury and may start showing up after a couple of weeks. That is what makes the head injuries such a sensitive subject.
Since head injuries could lead to several different conditions, it’s imperative to understand and diagnose if it’s a concussion before starting off with the treatment of the condition, even when a concussion is a prevalent type of head injury. The symptoms and signs can occur in some ways, such as physical symptoms, behavioral changes, irritability and moodiness, emotional signs and mental retardation. Here are the symptoms that are experienced by the patients with traumatic brain injuries or concussion.
- Commotion and confusion: Feeling confused due to the lack of cognition.
- Dizziness: Feeling dazed and disoriented
- Feeling clumsy: Lack of control over voluntary movement
- Difficulty in speaking: the patient can experience slurry speech due to neuropathic conditions and nerve damage.
- Feeling Nauseous: Vomiting and nausea can be experienced after a violent shock.
- A headache: persistent Headaches can be a symptom of damage to the brain.
- Difficulty in maintain equilibrium: due to dizziness and disorientation, it gets difficult to maintain balance.
- Blurred visions can also be associated with a head injury and concussions.
- The patient may also experience sensitivity to light and sensitivity to noise
- traumatic brain injury can make the patient sluggish
- A beeping or ringing sound in the back of the head.
- The patient may also experience emotional changes, behavior changes or changes in personality.
- A concussion can cause difficulty in focusing and retaining the concentration
- Memory loss is also a sign of a concussion.
Diagnosis for the traumatic brain Injury (Concussion)
The initial stages of diagnosis include an examination done by the doctor carefully in which the physical symptoms are noted, and the and the medical history of the patient is evaluated. Upon the onset of symptoms, the doctor will administer some neurological tests to ensure the condition. The signs and symptoms may take a few days to occur.
Depending on the types of symptoms experienced by the patient, the specialist will run one or more of the following tests:
Tests for Neurological symptoms
Physical examination will usually include testing for neurological symptoms. The doctor may examine the patient’s condition regarding hearing ability, vision, loss of balance, loss of reflexes, loss of coordination and cognition, loss of sensual perception, and the loss of core strength of the body.
Since the concussions are very closely related to the brain and its functional abilities, the specialist may also administer testing for cognition as a part of neurological examination, in which the patient’s evaluation will be based on their ability to focus and concentrate, the effectiveness of their memory and the ability to recall short term and long term information. CT scans for the bran may also be carried out by the doctor to identify the damage caused due to the injury. A CT Scan is a computerized cranial tomography test in which several X-ray tests are conducted to examine the bones of the skull. The Imaging of the brain for physical brain tests could be done if the doubts are well established. The doctors will also take notes for various symptoms related to concussion, such as seizures, swelling, persistent nausea, and headaches. The patient’s medical history is also examined as the part of the diagnosis. Since X-rays cannot singlehandedly identify the condition of brain tissues, an MRI may be administered to image the condition of brain issues and find the location of the damage for effective treatment.
Treatment for Concussion
After the tests show positive results and symptoms are apparent, the doctor may keep the patient under observation in the hospital or at home with someone to monitor if the symptoms alleviate or get worse. This would include checking on the patient again and again through the night to make sure that the patient can wake up from the sleep. If any abnormality is observed, emergency care would be required.
Rest is the most appropriate way to allow your brain to recover from a concussion. Your doctor will recommend that you physically and mentally rest to recover from a concussion. The patient should minimize or altogether avoid the activities that require physical exertion and too much activity, as a lot of exertion, wrong pressure and movement can reverse the healing and make the condition worse. The patient should avoid walking around and bearing any weights. It should also be ensured that the patient takes no mental pressure or stress of any kind, as it can also worsen the symptoms. If the patient is a student, activities that require mental exertion, concentration, focusing, and using too much brain power should also be avoided until things get back to normal. Entertainment activities that require mental and sensual involvement should also be avoided, such as watching movies, playing sports or video games, using a computer, doing homework, reading and using laptops or tablets. The best way to go about is to calm the mind and relax in nature.
If necessary, you will also be recommended to have shorter workdays and schooling, postpone homework, and take more breaks throughout the day. When the signs start showing improvement, the patient can gradually get back to carrying out their everyday activities that require mental and physical exertion. The specialist or doctor will make sure of when it is a good time for the patient to get back to life and continue with everyday activities. It will usually start by initially allowing the patient to do less rigorous exercises and training which requires less movement and jerking. Sports are highly recommended to be avoided for a long time after the injury, even when the patient recovers, as it can severely increase the risk of reversing the healing and causing a life-threatening injury. Medication can also be used to alleviate the symptoms that are causing trouble for the patient, such as pain, headaches, and bleeding.
Recovery & Effective measures after the injury
Concussions are not usually life-threatening as they are characterized as a kind of mild injury on the head. However, it doesn’t mean that the condition is not severe. Here are the things that you can do supplement the healing process and speed up recovery.
- Rest day and night
- Avoid highly demanding everyday physical activities
- Gradually start easy activities
- Visit your doctor for a checkup regularly
- Only use prescribed medication
- Avoid intoxication
- Eat healthy as it speeds up the recovery.
Groin Pull/Strain
What are Groin strains?
Groin strains can be defined as the injuries that are caused to the tendons and the muscles that result in palpation, pain and other symptoms. The proximal tendons such as adductor tendons and the injury to the bone can cause pain. Groin strains can be a common sports injury in many different games and athletic activities. The most common activities include soccer, football, ice hockey, running, tennis, rugby, American football, basketball and other similar games. It is the most common injury experienced by soccer players. Due to strong involvement of the adductor longus and such tendons in these games, groin strains can occur accidentally or when no prevention measures are taken. Usually, the damage is caused when the bone is inserted in the tendon accidentally.
A similar condition to groin strains is known as tendinosis. However, it is considered to be a gradually increasing chronic condition. On the other hand, groin strains are acute due to an injury of the localized myotendon connections.
The groin area covers the connection of the abdomen to both the legs through the pubis. The muscles of the groin can be classified into three types, the adductor group, abdominal group, and iliopsoas group.
- Adductors: there are six different muscles in this group.
- Abdominals: this group consists of three muscles.
- Iliopsoas: there are two main muscles in this group.
The most common group of tendons injured due to groin strains is the adductor group. The groin strains can cause a tear, avulsions, and contusions in the muscles. It can occur as a result of hip flexion and leg stretching. Depending on the severity of the contraction, the strength of the tendons, and the pressure put on the adductor, the tendons can get severely damaged and torn.
Categories of Groin strains
There are different grades for groin strains similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three grades are:
Grade 1: This is characterized by less than moderate pain, while the patient retains the ability to feel and move the injured area.
Grade 2: This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
Grade 3: This is characterized by severe pain, while the patient loses the ability to feel and move the injured area.
Causes of Groin Strains
There are many causes for groin strains that result from sports injuries. The most common causes include:
- Rigorous sports activities and movements
- Twisting of groin muscles
- Turning suddenly during a play
- A sudden strain due to kicking
- Running and stopping suddenly
- Continuing sports after mild strains and pain.
- An incorrect diagnosis from a previous injury.
- Repeated minor injuries
- Overuse syndrome
- Microtraumas
- Acute muscle hematoma of softer tissues
- Insertion of adductor tendons to bone.
- Chronic tendinitis
Types of Groin Strains
Groin strains can be classified into three different types:
- Repeated injuries
- Forced contraction
- Direct Blunt Trauma
- Symptoms for Groin Strains
- The result of groin strains can be painful and disabling. Here are some of the most common symptoms experienced due to groin strains:
- Tearing and disability of movement
- Tenderness of muscles in the groin, thigh, and spreading through the legs.
- Pain in muscles of the groin, thigh, and spreading through the legs.
- Pain in adduction movement and closing the legs
- Pain due to movement of the knee.
- Popping or snapping feeling
Diagnosis of Groin Strains
The diagnosis of groin strains is complicated and difficult, which is the reason why it can be easily mistaken as another syndrome. There isn’t any single best method for the diagnosis of the groin strains, as the muscle damaged and the conditions can vary among different patients greatly, and many other diseases, problems, and health conditions can result in a similar kind of a pain in the groin. Therefore, a differential diagnosis is administered to eliminate the possibilities of other conditions.
The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. If the adductors are damaged, the adduction movement of the thighs and legs become difficult and painful for the patient.
Once the initial examination is performed, and the doubts are reduced, the doctor may follow up with diagnostic procedures. The techniques used in this case are radiographic investigations, ultrasonography, the differential diagnosis, and sonographic evaluations. If necessary, the doctor may also use MRI scans to find out the exact location of the damage.
From acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine position, and the movement and flexion of the hip and legs are examined.
The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain, tenderness of the abdominal, adductor and the iliopsoas tendons.
Treatment for Groin Strains
The treatment can be administered in different ways. One of the most common treatment is rest, ice, compression, known as RICE procedure. The very first response should be immediate first-aid care to alleviate the symptoms of pain and swelling. After the diagnosis, the doctor will assign to you an easy to follow the treatment plan that you can practice at home.
Exercises
The injuries related to groin strains can be treated with the help of proper exercises that are administered under the supervision of a doctor or a physical therapist. Some different simple exercises can be helpful. In most cases, the problem of groin strains can be solved within one or two days after a person experiences an injury. The approach of these exercises is to stop the bleeding, reduce the swelling if there is any, and to alleviate the pain in the injured part to ease the patient.
The first approach to treatment is resting the leg as much as possible. The patient should avoid walking unless it’s necessary and physical therapy should regularly be administered. The patient shouldn’t move the injured area and keep it still as much as possible.
To avoid stiffness, careful movement of the leg should be gently done every two days. For raising the leg, the patient should use a footstool or other aid.
To avoid swelling and alleviating pain, icing can be done by the patient according to the advice of the doctor. For that purpose, Ice pads and ice packs can be used to soothe the injured area. In case if regular ice is not available, the patient may also use a pack of refrigerator items which is frozen, such as frozen peas. It’s important to know that the patient should not put ice on the injured area directly, as the direct contact of ice with the skin can cause burning, referred to as ice burning. The best practice is to ice the injured area after 2 hours throughout the day. For each icing session, the patient should ice the injured area gently for as long as 20 minutes.
Another approach for treating this problem is compression technique. This technique involves compressing the area which is injured for alleviating the pain and reducing the swelling. This compression can be done by bandaging the injured area tightly at the right place on the thigh. This may be very effective for most cases, and may not work for some patients depending on the area, type and severity of the injury. That’s why it’s important that an expert person who is trained to do this should be consulted, as experts know better about where and how to tie the bandage.
Medication can also be used for the injuries related to groin strains. These may include painkillers and other drugs that can help treat the swelling and provide relief. Some OTC drugs are available in the market which should be used according to the prescription of the doctor.
Physical therapy is another effective method for the treatment of groin strains. This is effective not only at the time of acute trauma, but it can also be used continually for an extended period as a rehabilitation response to the injury. This treatment requires the supervision of an expert and trained physical therapist who will examine your condition and decide which exercises are suitable for you. Each patient may have to go through different physical therapy. Therefore, it’s essential to get a proper examination of your condition before moving on with the therapy. Once your physical therapist finalizes the right kind of exercises for you, he may give you an exercising routine which you can follow on your own on a regular basis. The approach of physical therapy is to restore the affected movement of the leg and to improve the body’s capacity to ensure quicker healing and speedy recovery. Following the right treatment plan can make a significant difference regarding healing time and effectiveness. Apart from the exercises involved in your physical therapies, you may also be able to benefit from the massages of the injured area. These massages are aimed to soothe the soft tissues associated with the injured area which can improve the blood flow and ensure a quicker recovery. For this purpose, you can count on your physical therapist and learn the right approach from him to practice it on your own later on.
Here are some of the most effective and easy exercises that you can try for the treatment of groin strains. However, you must understand that some of them may not be suitable for you and you should consider these after advising from your physical therapist or a doctor.
These exercises may be continued at least two days after the injury. During that time you should allow your injured area to rest as much as possible. It’s important to keep these exercises simple and on point.
Floor stretches
Floor stretches are done by lying on the floor straight on your back with your legs stretched. Legs are moved by stretching them outwards from the body posture one by one after returning each leg to the original position before moving the other.
Chairlift
Chairlift exercise can also help in some cases. It can be done by sitting on a chair with your knees bent, and slowly lifting each foot as high as your ankle is lifted to your groin level. The lifted foot should be kept that way for a few seconds before putting it down and doing the same thing with the other foot.
Knee Squeeze
As the name suggests, knee squeeze exercise involves a movement of the knee to squeeze a soft object. It is done in a sitting position and placing a soft rolled towel or a ball between the knees while holding it. Press your knees together to squeeze it for a few seconds before releasing the squeeze. This involves using the muscles that are stretched up to the groin area.
Apart from exercises, you must rest as much as possible and avoid a lot of activity. In severe cases, you may also use steroid based medication. However, the use of it is discouraged unless it’s absolutely necessary for treatment and recovery. Some severe conditions may also require surgery or operation, such as adductor tenotomy. Each type of treatment option may involve a post-treatment rehabilitation therapy in most cases.
Here is a quick to-do list for the treatment:
- Resting as much as possible
- Icing the painful area and between the legs
- Using compression bandages
- Anti-inflammatory medication
- Exercising, stretching, friendly workouts
- Gradually start physical activities, don’t rush.
- Surgery as a last resort, if no results and symptoms persist after the treatment.
Prevention from Groin Strains
Prevention is always better than care. Several preventive measures should be understood and exercised in the fields. The best way to go about it is to practice them during the training until they become your reflexes. The prevention measures can be classified as primary and secondary preventions, and both of them are very important. The risk factors associated with groin strains should also be addressed and taken care of, including the patient’s history of groin strains, the strength of the muscles and the previous injuries. The patients who have experienced previous injuries are two times more susceptible to experience it again upon a heavy blow, while the risk of groin strains in people with lesser strength in the adductor tendons is quadruple.
These risks can be minimized by taking the rehabilitation therapy seriously. If the previous injury is not healed completely, there is an excellent chance that the little healing that is done will be reversed and the same acute condition will occur again. This can also make the region very week and easily injured again and again. Muscular exercises and workout that focuses on strengthening the core muscles and the tendons are very effective to build strength and endure pressures on such area. These include several core strengthening exercises, adduction exercises, coordination practices, skating and sliding workouts, and balancing practices.
Here is a brief checklist of the preventive measures:
- Sufficient warming up of groin and legs before rigorous sporting, running, and activities.
- Use the right footwear
- Start off slow, and gradually improve and intensify your exertion.
- Don’t continue exertion after pain and stiffness in the area.
- Exercise regularly and keep your body used to exertion and pressure.
Recovery from Groin Strain
Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area and other factors. Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. For effective recovery, you should get back to the usual routine activities slowly and gradually according to your doctor’s advice. Once you start using your muscles and bones again, it will complement the complete healing of the injured parts. If the patient were healthy before the injury, the recovery would usually be faster. However, due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the injury can take from a few weeks to 6 months of time to recover.
Here is what you can do to ensure speedy recovery:
- Rest day and night
- Avoid highly demanding everyday physical activities
- Gradually start easy activities
- Visit your doctor for a checkup regularly
- Only use prescribed medication
- Avoid intoxication
- Eat healthy as it speeds up the recovery
SHIN SPLINTS
What are Shin Splints?
Shin splints can be defined as a condition of acute pain in the leg and shin area which is caused due to overuse, overexertion, or prolonged running on the hard ground. It can result in a throbbing and aching condition after a sprint. In medical terms, shin splints are also called as medial tibial stress syndrome based on the muscles affected by it. Due to acute stress on the muscles and tissues located in the thigh bones and shin, pain, swelling, and inflammation can occur.
Shin splints can be considered as one of the most common types of repetitive strain injury experienced by the athletes and sportsmen. A variety of conditions can be defined as shin splints. The most common shin splint conditions are medial tibial stress syndrome, compartment syndrome, and the tibial stress fracture. Medial tibial stress syndrome is the most common type of shin splint, and it’s characterized by the degeneration of the shin bone, irritation and the damage to the muscles and soft tissues around it. The myofascial trigger points are the muscle knots in the anterior tibial muscles which can often remain undiagnosed and untreated. Due to these complications, the wrong treatments and diagnosis may be administered to the patient.
Risk Factors for Bursitis
Age is one of the most critical risk factors for bursitis. People involved in sports who are older than 30 years are more at risk of getting a Bursitis inflammation. Apart from that the type of sports and the strength of tendons and muscles also have a significant amount of determining the impact on the risk of bursitis.
Symptoms of Bursitis
Pain is the most important symptom of bursitis which can be aggravated by the movement. The pain can either be chronic or develop gradually over a long term, or it can be due to a sudden injury or blow. Difficulty or complete loss of movement ability is also experienced by the people suffering from bursitis. One such condition is known as adhesive capsulitis when it happens to the shoulder. As a result, the shoulder gets frozen and cannot be moved. Occasionally the patient may also experience swelling, redness, and warming of the injured area. The symptoms you should generally look for are the following:
- Feeling pain and stiffness
- Increased pain occurring due to movement or compression
- Redness and swelling.
- Difficulty or inability of moving joint due to pain
- Bruising and rashes
- Sharp and stinging pain during exercising
- Feeling feverish
Treatment for bursitis
Bursitis treatment may have different approaches depending on the severity of the condition and the type of pain the treatment method is chosen to be administered. This also involves the type of structure and the part of the body that is suffering from bursitis. Preventive measures, as well as proper care, can significantly factor in for the effective treatment. The pain and swelling should be addressed first, and it should be ensured that there is no bleeding as a first aid response. In the long run, your doctor will guide you through with some treatment plans to cure the condition.
Bursitis treatment also involves the consideration of infection along with the condition. The treatment is chosen based on the presence or absence of infection along with bursitis. Bursitis that occurs with an infection is referred to as septic bursitis, while the one that occurs without an infection is called as aseptic bursitis. In the case of non-infectious or aseptic bursitis, some treatment options can be administered. The most commonly administered treatments are anti-inflammatory drugs, compression, rest and pain relieving medicines. These techniques can effectively reduce the symptoms and help speed up the recovery. The patient may also require bursa fluid aspiration in some cases. For that purpose, a syringe is used with a sharp needle to remove the fluid. It is done by an expert as it requires several sanitation and other considerations. It is usually done in the clinic or the doctor’s office. The fluid is retrieved, and it is forwarded to the labs for analyzing the conditions. The bursitis cases involving non-infectious conditions, the doctor may treat the patient under the action of anesthesia. The cortisone injectables are used for the treatment, and it is administered in the swollen area of the injured bursa. The chemical substance is very active and provides quick results. It can also recover the patient in a matter of a few days in most cases. This injection procedure can be carried out in combination with other treatments, such as the bursa fluid aspiration procedure. Apart from these options, you may also use other medication, NSAIDs and over the counter drugs. The most commonly used drugs in this regard are Motrin, Advil, Tylenol, and Aleve.
The treatment of bursitis may also involve other secondary aids. The patient can use braces and crutches. Moreover, the bursitis patients can also benefit from wearing footwears that are proper for bursitis as a preventive measure and to ensure that healing is accelerated. Other approaches can be incorporated in the treatment, such as weight reduction.
Exercising is also important to keep up with a healthy treatment regime. These involve stretching exercises which can prevent the patient from stiffness. The patient should be careful while choosing the exercises and they should be administered under the supervision of a physical therapist or a doctor. The patient should also avoid climbing the stairs and walking on uneven, hilly and rough surfaces. You should also avoid walking on steep surfaces. Some anti-inflammatory exercises may include Stairmaster and other such exercises.
Septic bursitis or infectious bursitis requires a more thorough approach because of the infection. The condition is rare, and it may require a surgical fixture of the problem by draining the infected bursa fluid using the technique of bursectomy.
Some of your lifestyle habits may also be responsible for a bursitis condition. That is why it’s important to take corrective measures regarding the things you may be doing wrong that caused bursitis. For this purpose, you can consult a physical therapist who will evaluate your lifestyle to observe the things that you might be doing wrong. You should also adopt an anti-inflammatory lifestyle which can help you effectively avoid inflammatory conditions. Some of the best ways to go about the treatment of bursitis are:
- Resting as much as possible
- Icing the painful area
- Using compression bandages
- Anti-inflammatory medication
- Exercising, stretching, friendly workouts
- Physical Therapy
- Gradually start physical activities, don’t rush.
- Surgery if no results are seen, and symptoms persist after the treatment.
Preventive measures for Bursitis
People who are not used to exercising and rigorous movement are more at risk of developing a bursitis condition. As a preventive measure, you should keep up with your exercising and work out regime to avoid any sudden damage to your muscles and tendons. Training can help make the tendons and muscles more flexible and robust. As a result, the impact of the injury can be minimized. In case if you already have a pain in particular part of your body, you should avoid training and sporting until the pain gets better. Otherwise, the pain can get worse with exertion and lead to a more severe condition. If you feel an onset of pain while playing or training, you should stop instead of ignoring it and continuing with your activity. Certain types of bursitis are not preventable. However, there are certain things that you can do to minimize the risk of bursitis, such as:
- Using the particular type of padding to decrease the compression and pressure
- Correctly lifting weights and take preventive training measures
- Not lifting heavy loads on your back
- Taking more breaks whenever your body asks for it
- Preventing obesity as it can increase the risk of bursitis.
- Making your muscles and joints stronger by exercising and training.
- Always making sure that you do stretching and a warm up before training and exercising.
Fractures
What are Fractures?
The term Fracture means a break in medical terms. Generally, the fracture is used to refer to the break in any bone in our body. However, in everyday language, the term is also used as muscle fracture to indicate the twisting, polling and spraining of the muscles. There are many reasons why fracture is characterized by a very severe injury or health condition. The injury causing fractures can be excruciating in most cases. A break in the bone can be healed naturally, for which some aids such as crutches and plasters are used to keep the broken bone into its right place. An average human adult has 206 different bones in their body. Therefore, there are numerous possibilities of a fracture, and it can be classified into different types. The most common fractures are experienced in the limbs, arms, legs, ribs, fingers, and jaw. In some different sports, the fracture is one of the most common sports injuries, as certain sports can be rough. However, preventive measures and right training can significantly minimize the risk of fractures in athletes and people involved in sports.
Symptoms of a Fracture
A fracture is a serious injury; the condition can lead to severe and sudden pain. Broken bones also damage the tissues, muscles, and tendons that are serving the covering purposes. Usually, it’s easy to identify that an injury has caused a fracture as the symptoms are usually very evident. However, sometimes a physical examination, as well as the diagnostic tests, may be needed to make sure that it’s a fracture. The common symptoms that occur with fractures are swelling, bruising, and discoloration of the skin, inability to move the injured area, tenderness, evident bone displacement, obvious deformity, and a lot of pain. Depending on the type and the location of the fracture, the symptoms may be different.
Other common symptoms may include:
- Bruising and discoloration
- Angulation and bending of the affected area.
- Inability to bear weight on the injured bone
- Inability to move the injured bone
- A feeling and sound of grating sensation
- Bleeding in case of open fractures.
- Severe and larger fracture can cause paleness
- dizziness
- feeling nauseous
Different Types of Fracture
Fractures can occur due to a variety of different causes in people who are involved in sports. Usually, it’s due to a heavy blow, falling, or a severe traumatic injury. Sometimes the fracture can also result from overuse, repetition of the movement and put too much stress and pressure on the area. Depending on the location and the severity of the fracture, it can be classified into different types. The simplest classification puts it into two distinct groups, known as the closed fracture of the compound or open fracture. The first type is a lot more common in cases of sports injury, and under these conditions, the skin is not torn, and the fracture happens internally. In case of open fracture, due to the breakage, the broken bone can poke out from the skin causing bleeding and severe muscular damage.
Regarding other classifications, the fractures can be classified into several groups, such as:
Transverse fractures: this type of fractures are characterized by a straight line as of breakage.
Avulsion fractures: avulsion occurs when muscle tearing can pull apart a piece of bone along with it.
Comminuted fractures: it can be simply understood as multiple fractures on a single bone.
Spiral fractures: in this type, a spiral breakage is formed around the bone.
Oblique fracture: as the name suggests, this second type of causes a diagonal split of a bone
Compression fracture: this type results from a fracture in spongy and soft bones upon compression and pressure.
Fracture dislocation: this type causes dislocation of the joint.
Greenstick fracture: in this type of fracture, the bone only breaks partially. This means that it’s not a complete fracture, and only one side of the bone is cracked.
Hairline fracture: this type is difficult to diagnose even with X-rays as the split is as thin as a hair. In several cases, it is left unnoticed.
Impacted fracture: a fracture of one bone due to the piercing of another fractured bone in it can cause impacted fractures.
Intraarticular fracture: this fracture occurs on the bone, and it’s extended towards the joint with another bone.
Longitudinal fracture: in this type of fracture the length of the bone is affected.
Pathological fracture: pathological fractures can occur as a result of another underlying health condition or a disease that is causing the weakening of the bones, such as osteoporosis.
Stress fracture: due to the repetition of the movement and persistent stress, a fracture can be caused.
Buckle fracture: it results in bone deformity instead of an actual split.
Complications of Fractures
A post fracture treatment requires proper healing and the enjoining of the broken segments of the bone. However, if this does not happen properly, it can result in a bone deformity and displacement. Sometimes fractures can also result in infections typically in the open fractures type where the skin is torn. The possibility of infections is eliminated by administering the precautionary measures and antibiotics. In the majority of cases, fractures can cause damage to the proximal tissues and softer muscles located on or near the broken bone. It can also damage the nerves, the tendons, ligaments, and the blood vessels. The symptoms of fractures may get worse gradually with the passage of time. If proper measures are not taken, and the condition is ignored, it can develop into serious complications. Fractures can also result in muscle wasting in most cases. The death of proximal muscles may be caused due to fractures. Proper therapy can reduce the risk of this problem. Another complication, as well as a risk factor involved in cases of fractures, is the deep vein thrombosis. To avoid such complications, it’s best to follow a strict physical therapy and maintain the blood circulation.
How is a Fracture diagnosed?
The diagnosis for fracture can be a thorough procedure in certain cases. However, in many cases, it is quite evident just by looking that it’s a fracture. The patient is also mostly able to tell if the pain is muscular or if it’s in the bone. Sometimes muscular damage can also occur due to a fracture, which can cause confusions. Since there are some different fractures that various parts of our body are susceptible to, sometimes they can be extremely severe and difficult to handle. Things can get very complicated, and the condition can become extremely persistent. Nonetheless, the primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain, the inability of movement, bone condition, and swelling. The doctor may also carefully examine by moving the bone and the joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an X-ray diagnostic test to identify the bone condition, an ultrasound test or an MRI (magnetic resonance imaging) test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound can sometimes help the doctor to locate and study the internal structures to see any possible damage.
Treatment for the Fractures
Fractured bones usually recover and help through a natural procedure. However, the recovery can be supplemented by eating healthy, resting the fractured area as much as possible and taking supplements such as calcium and vitamin D.
The most important part of the treatment process is ensuring the healing is supplemented with the help of aids to ensure that the location and placement of the healing bones are kept perfectly to avoid any dislocation or deformities. It is focused on ensuring that the most suitable and optimal conditions are provided for allowing the bone to heal properly and promptly. This is usually achieved by administering a variety of ways to cause immobilization of the area.
The treatment starts with the lining up of the broken bones bringing them together as one unit. The process is called reducing the fracture as it brings the fractured bone closer together. This procedure is carried out under the effect of anesthesia which causes the patient to sleep in most cases as the process can be very painful. Surgery may be done to achieve this purpose if the case is severe. After the alignment, a variety of techniques may be used for the immobilization of the fractured bone, such as:
Plasters and braces- these are used to hold the bone exactly in the same position for a couple of weeks or even months. After the healing, it’s cut with the help of a saw.
Metal plates and screws – screwing and putting metal plates can keep the bone into place.
Intra-medullary nails – nails or rods are used on the larger bones and wires are used to hold the bone into place.
External fixators – this uses scaffolding technique by internally placing the carbon fiber directly into the bones.
The immobilized procedure is required for as much as two months in severe cases. During this period, the patient practices self-care practices and other complication may be monitored. It results in a simple healing process as the bone cells merge into each other by absorbing the old cells and producing the newer ones. A new bone may be formed, which is called a callus.
Physical therapy
After healing, a physical therapy remains to be a very effective treatment for the conditions of fractures. It can ensure the proper placement of muscles, bone and the joint, improve the strength and enhance the flexibility of the muscles and the tendons that surround the fractured bone. The condition can be developed in an acute manner as well as in a continuous and gradual manner. A single heavy blow, jerk or an injury can result in the fracture, of the tendons and muscles may get deteriorated over time by repetitive and smaller injuries.
Surgery: Plastic surgery may be administered to heal the damaged skin and muscles. However, in certain cases, a surgical procedure may be required for the alignment for the immobilization technique.
Preventive measures for a Fracture
There are certainly a number of different ways in which we can ensure that a fracture is prevented. Sports can leave a person susceptible to an accident. However, taking proper measures and training can help a person in protecting himself even when he experiences an accident.
Here are some of the most effective ways to prevent a fracture:
- Ensuring the bone health by eating healthy
- Wearing the right suits for the sports, including paddings, etc.
- Training to strengthen the bones and the muscles surrounding the bones
- Stretching and regularly flexing along with the workout
- Ensuring calcium and vitamin D intake to strengthen the bones
- Preventing the direct impact of stress and pressure on the softer bones at the time of an accident
- Treating any underlying health conditions which may weaken the bones, such as osteoporosis, osteogenesis, osteoarthritis, and cancer.
- Preventing oneself from falls and accidents
- Ensuring muscular health to avoid avulsion fractures
Muscular cramps
What are Muscular Cramps?
A muscle cramp is a very common condition in the sports injuries which is characterized by a strong and very painful contraction or tightening of a muscle. The condition usually occurs all of a sudden, and it may continue for a few seconds or several minutes. In most cases, muscle cramps take place in the leg, feet or thigh area. The condition is also known as charley horse in common terminology. Sometimes the muscular cramps can occur during the night as a result of muscular spasms, muscular loosening and tightening as the person relaxes. It can also be experienced by people involved in sports. Therefore, it can occur both due to a lack of activity as well as too much vigorous activity. Most of us get muscular cramps at some point in our lives, so it’s quite a common condition. It results from forced contraction of the muscles which is involuntary. The causes of muscle cramps are numerous, and so are the types of muscle cramps. However, we will focus more on the causes related to the sports arena. It can occur due to the muscular contraction during a workout or exercise, and it can also occur when a person is relaxing. Each type of muscle cramp is associated with a cause. In the case of people involved in sports, they can be prone to dehydration as sports can cause too much perspiration. Therefore, dehydration is also a very common cause of muscle cramps in sports people and athletes. There are several medications as well that can result in muscle cramps as a side effect, and it’s usually written in the side effects of those medicines. In certain cases, the muscle cramps can be excruciatingly painful, and the patient may scream out of pain, and it can even last for as much as 45 minutes. Cramping of other involuntary muscles is also possible, such as the bowels, blood vessels, uterus, urinary tract, and bronchus. However, we will focus on the cramps that involve a musculoskeletal system of the human body, as these are the ones that are mostly associated with sports.
Although the condition is not a very serious issue, it can be really painful and uncomfortable at times. A person who is prone to muscle cramps may experience cramping repeatedly and frequently. That is why a proper treatment is advice for those people to eliminate the problem completely. The cramps of the muscles can be stopped if it’s possible to allow the stretching of the muscles. It can the muscle stretching is not possible, it can be difficult to address this problem sometimes. However, it’s mostly a condition that ends itself, and the person can get back to normal instantly. There are a number of things that we can do to prevent it from happening and to alleviate the pain at the time of a cramp. There are a number of factors that can increase the possibilities of a muscle cramp. Some of the factors that are in our control include a healthy and proper diet, healthy lifestyle and activities, and adequate stretching, workout and exercising. A person involved in sports should also care about keeping himself hydrated at all times not only to prevent muscle cramps but also to ensure overall body health in a number of different ways.
Risk Factors for Muscular Cramps
- Being inactive
- Lack of exercise
- Being older
- Being a female
- Pregnancy
- Dehydration
- Improper training
- The type of sports
- The type of medicines taken
Types of muscle cramps in sports injuries
There are several different types of muscle cramps. However, sports injuries and sports related muscle cramps as associated with the musculoskeletal system of our body. Therefore, the relevant types of cramps are important to us. The musculoskeletal muscle cramps can be classified into four major types, including the true cramps, dystonic cramps, contractures, and the tetany cramps. The classification is based on the types of the cramps, the underlying causes for the cramps, and the area of the affected region.
True cramps are the most common type of muscular cramps experienced in sports people and athletes. They can be experienced in a part of a group of different muscles that function in combination. Such muscles include the flexion muscles of the legs and fingers. The most common cause of true cramps is considered to be a simulation of the muscles and the hyperexcitation of the nerves involved in them. It can be a result of injury and cause persistent muscular spasms. It can be considered as a reflexive response of the muscles to resist the impact of injuries to the muscles and the bones, such as in case of a fracture. It causes inability or serious limitation of the movement of the injured area, stabilization of the injured part and muscular spasming. These cramps can also result from vigorous activities involved in many sports. It can be a result of fatigue, overuse, and overexertion of certain muscles. Another reason for such cramps is resting, which is experienced by aged sports people. It usually occurs during the night and causes a severely painful condition. Dehydration can also cause serious cramping for the sportsmen and athletes as a result of heatstroke or excessive perspiration. Such cramps may also be caused due to the low levels of magnesium, potassium, and calcium in the bodies of people involved in sports. Body fluid imbalances can also result in muscular cramps.
Another type of muscular cramps is tetany cramps, which are caused due to the stimulation of the muscles and the excitation and activation of the proximal nerves. It may cause cramping in all the body. Sometimes it can be difficult to differentiate tetany cramps from true cramps.
Dystonic cramps are caused due to the contraction of muscles that are not meant or intended to be moved. It usually includes the cramping of muscles that work in the opposite direction. This is a less common type and occurs in smaller muscles. It can also be a result of overexertion and fatigue.
Contracture is the fourth type of cramping. However, it is not an actual type of cramping. In fact, it’s a distinguishable condition that can be mistaken as cramping. It is a condition characterized by scarring of the softer muscles and tissues involved in the muscular movement. As a result, the movement of the muscles is limited with the onset of pain.
Causes of Muscle Cramps
Muscular cramps can occur out of the blue and very suddenly. However, there is always an underlying cause for the condition. The causes differ from patient to patient and greatly determines the type of the cramp and the condition the patient is expected to experience. Although there are several causes for muscular cramps, the most common causes of muscle cramps are:
- Fatigue of the muscles
- Overexertion of muscles
- Pain in the affected area
- The weakness of the muscles
- Inactivity
- Vomiting can cause cramps
- Lethargy and exhaustion
- Sudden Weight Loss
- Swelling of the muscles
- Difficulty in breathing
- Confusion during movement
- Lack of the muscles’ strength
- Fever can cause cramps
- Medication
- Deficiency of vitamins and minerals
- Poor blood circulation
Diagnosis of muscle cramps
Physical examination is performed for the diagnosis. The symptoms are observed in the physical examination stage. These symptoms include:
- Inability to use and move the injured area
- Persistent Swelling
- Soreness
- Bulging due to muscle knotting
- The firmness of the muscles
- Tenderness
- Mild to severe Pain
If these symptoms are observed, the diagnosis indicates the possibility of muscle cramps. Although there aren’t any specific diagnostic tests for muscle cramps, they aren’t required either since it is comparatively easy to diagnose a muscular cramp. In most cases, the patient himself is aware that he is experiencing a muscular cramp, and the doctor can endorse the doubt.
Treatments for muscle cramps
Stretching of the muscles is a good way to stop and treat a muscle cramp condition. The stretching can be done by softly allowing the muscles to move and function in the proper way they’re meant to function. For instance, in the case of leg cramps, standing, flexing and walking around can help alleviate the condition. Moving the leg in different directions to find the most comfortable spot can also help alleviate pain and stretch the muscle. The stretching is usually more about common sense, and the patient can understand what is needed to be done with a little knowledge and interaction with the pain. Similarly, calf cramps can be treated by standing close to the wall and leaning towards the wall and stretching. These techniques can be easily learned with a short tutorial. The cramps can also be treated by massaging the muscles in certain cases. Massage oil can be used for the treatment. Medication is usually not required neither prescribed because the cramps are self-ending in most cases and they will be gone even before the medicine starts to absorb and act. However, if absolutely required, certain muscle relaxants can be administered to soothe and relax the muscles that are experiencing cramping temporarily. Latest medicines are also using Botox toxin and injectable to treat severe cramping conditions. However, this remains aloof from the scope of sports injuries.
Preventive measures for Muscular Cramps
Almost everyone is bound to experience cramps at some point in their life. Therefore, the best approach is to prevent it from happening. There are certain things that you can do to minimize the risk of cramps, such as:
- Stretching before starting activities, sports, and exercise
- Warming up and cooling down
- Keeping yourself hydrated at all times
- Avoid overexertion and fatigue
- Keep electrolytic balance
- Keep up with vitamins and minerals
- Avoid excessive weight loss
Delayed onset muscle soreness
What is Delayed Onset Muscle Soreness?
Delayed onset muscle soreness is a condition that is often referred to as DOMS. This condition is especially characterized by the symptoms of the pain and the stiffness in the muscles which can last from several hours to several days after going through rigorous training or exercises which the body is usually not accustomed to. It’s a very common condition experienced by people in sports, athletes, people who train and gym, and newcomers to heavy training.
The more we train, the more our muscles get strong. However, if your muscles are not used to heavy exertion, you must start slow and gradually increase the training. Otherwise, too much stress and pressure on your tender muscles all of a sudden will definitely cause muscle fatigue, overexertion, wearing and tearing of the muscles. This can result in soreness that can last for up to 4 days depending on the severity of the condition. This condition is extremely common as almost every second or even first person will experience delayed onset muscle soreness after their first heavy workout. Therefore, this is where proper guidance by your trainer comes in handy. The reason behind it is so common is that the symptoms, stiffness, and pain start building up gradually a while after you’re done with your workout. During the workout, our body remains warmed up, and we are not aware of the threshold capacity of our muscles. As a result, in the phase of it, sportspeople usually end up doing it out of enthusiasm. However, it will do more harm than good. That’s why doing less is better than overdoing it during your first few sessions.
DOMS is considered to be a result of muscular lengthening exercises which can cause micro damages to the muscles, often referred to as microtrauma of the muscular fibers. In simple terms, the muscle fibers break and heal again. This breakage can cause pain, stiffness, and the inability to move them. It doesn’t mean that this breakage is not required. That is how our muscles build up stronger after healing. However, it needs to happen gradually and slowly. If the pain from the DOMS is mild and the patient continues the exercise, it can get more severe. Therefore, it’s recommended to rest until the pain is gone. Delayed onset muscle soreness can also be a condition as a symptom of muscular damage caused due to exercising and training. Although the pain is not evident during the workout when the body is warm, the condition starts to show up once the body temperature drops and the body cools down.
Signs and symptoms of Delayed Onset Muscle Soreness
Pain is the most important symptom of DOMs which is usually accompanied by the stiffness of the muscles. Apart from these symptoms, other common symptoms include muscular soreness, a dull and aching pain, sometimes a swelling, tenderness of the muscles, pain upon touch and a feeling of palpation. There may be particular positions and angles in which the perceived pain is minimized, and the pain can increase if the damaged muscles are contracted, stretched, pressurized stressed and moved. Muscular tenderness is among the common symptoms and in this condition is it known as mechanical hyperalgesia of the muscles. The soreness and pain can remain for up to a week depending on the severity. However, it is maximum during the first four days, with the exception of the first day when pain gradually starts building up.
Causes of Delayed Onset Muscle Soreness
The causes are usually the same in the majority of the cases. Some of the most common causes associated with DOMS are as under:
- eccentric exercise (lengthening exercise)
- muscular contractions during exercises
- static or isometric exercises
- overexertion during workout
- working out for more than 1 hour without warming up
- Starting off with heavy training all of a sudden.
Preventive measures for Delayed Onset Muscle Soreness
Depending on the causes of Delayed onset muscle soreness, we have the most control over protecting ourselves from it and preventing the DOMS Condition from happening. It is not likely to be caused due to an accident, and in most cases, it is due to the behavior, habits and the mistakes of the patient. Here are some of the most effective things you can do to prevent DOMS from happening:
- Avoid intense workout at the starting
- Gradually increase the workout time and intensity
- Make use of the repeated-bout effect
- Limit the concentric and static types of exercises
- Avoid muscular fatigue
- Avoid overstretching in the name of warming up
- Limit the movement range and stretching during the workout
- Use the correctly fitted compression garments
- Eat healthy and nutritious
- Keep electrolytic balance
- Keep up with vitamins and minerals intake
- Use Turmeric in a routine with the workout
Treatment for the Delayed Onset Muscle Soreness
There are certain measures that can be taken to reduce the condition and treat it. The most important treatment is taking proper rest to ensure that the body gets enough time to heal the muscles and avoid the damage from further exercising. In most cases, you’ll be good for a couple of days, so there isn’t much to worry about. However, it shouldn’t be underestimated, and proper care should be administered. Even if the injury is less severe and you don’t take proper care, it can worsen with further mistakes. So reduce your intense activities as much as possible for the time being. Although not necessary in mild soreness, but sometimes the PRICE treatment can give significant and effective results especially when the condition is severe. Gentle massages for the issue of DOMS can be very effective due to the nature of the problem. A soft, gentle massage will help improve the circulation of the blood in the area and speed up the healing of the damaged muscles. This healing can be accelerated by eating foods that fight inflammation and have healing properties. Turmeric, also known as curcumin is also a magic ingredient which has amazing healing properties. So, make sure that you use that. Hot baths can also help alleviate the pain and soreness, so don’t hesitate to try sauna. Massages, on the other hand, can increase the overall blood flow in the region and help speed up the recovery. Another approach to take for alleviating the symptoms is resting, Icing, compression, and elevation can also help in to reduce the symptoms. Resting is the most important part of the healing process, as a wrong pressure and movement can reverse the process of healing and make the DOMS condition worse. Furthermore, icing can be done for 20 minutes to 30 minutes a number of times throughout the day for a few days until the symptoms are eliminated. The sore muscles can also be compressed by compression bands and fastening an elastic wrap around it. The pressure should be moderate to avoid any excess strain on the area. The recovery time for DOMS may range from a few days to a few weeks. Although it’s not recommended to exercise rigorously, it’s also suggested to not get into a rest phase entirely. Exercising can actually help alleviate or at least suppress the pain to some extent if you know how to do it right. You certainly don’t have to do a lot of stretching and worsen your condition. This effect is known as exercise-induced analgesia. Some people do consider it the best way to alleviate the soreness. However, it cannot be endorsed scientifically. Therefore, it’s better to stick with the conventional plan, as the condition will eventually be treated in a matter of days in most cases. Your plan should overall include:
- Taking a break from the normal exercise routine
- Stay limber with your exercising and practice light exercising
- Physical therapies like RICE and massaging
- Eat and drink healthy
- Try anti-inflammatory medication in severe cases
- See a doctor if needed
Frozen shoulder
What is Frozen Shoulder?
Frozen shoulder is a common condition in sports injuries which is characterized by pain and stiffness in the shoulder joint. In medical terms, it is also known as adhesive capsulitis. It is one of the most common shoulder injuries. However, unlike other injuries, the condition can persist for a long time and may even remain a problem for three years. The symptoms usually start to begin gradually with an initial onset of discomfort, which gradually turns into mild pain and then starts getting severe. This is one reason why it’s important to limit or even stop exertion and rigorous activities if the shoulder joint starts to show mild symptoms. This should be followed by a proper treatment plan. The treatment for the problem of frozen shoulder in most cases requires very thorough and aggressive treatment in a number of ways. In severe cases, medication and injectable are also required. The medication usually includes anti-inflammatory drugs, and the injections are needed to be administered on the shoulder area, such as cortisone injections. Apart from these methods, physical therapy is also essential for an effective treatment of frozen shoulder. There is intensive care needed in the treatment of the frozen shoulder as the condition can become permanent if proper measures are not taken and if the condition is repetitively ignored. The problem can sometimes show excessive resistance to various treatment methods. Therefore, this is a problem that all the people involved in sports should be aware of. Other underlying conditions can also increase the risk of getting a frozen shoulder, such as a mastectomy or a stroke. Usually, the treatments which require the patient to limit the movement of the arm can increase the risk of frozen shoulder. The condition can also be mistaken with other conditions, such as arthritis. However, this is a totally different and unrelated condition.
There can be a number of ways to treat this condition, and in most cases, it will require a combination of several effective treatments. Steroid drugs may also be required in cases of severe injuries. However, it’s usually avoided due to the heavy side effects. If the problem persists, surgical procedures may be required to treat the condition. The most common surgical procedure administered for the treatment of frozen shoulder is arthroscopic surgery. A number of complications may also be experienced by the patient. The most common complication is the recurrence of the frozen shoulder problem on the same shoulder even after the complete treatment is administered. However, the second frozen shoulder can be experienced on the opposite shoulder as well.
Symptoms of Frozen Shoulder
The symptoms of the frozen shoulder may vary from patient to patient depending on the severity of the condition and the time period for which the problem has existed. The symptoms start to build up gradually, and the problem can span three stages. On each stage, the problem can persist for months before entering the next stage.
First Stage: The first stage for a frozen shoulder can be considered as a Freezing stage. As the name suggests, it completely disables the movement of the shoulder and can cause severe pain. The condition starts building up gradually, first with a limitation of the full range movement, which slowly develops into complete freezing.
Second Stage: The second stage can be considered as the frozen stage. This stage begins at the end of the first stage when the shoulder movement is disabled to the maximum. The stiffness is maximized at this stage. However, the pain in the shoulder starts to get duller gradually. The
Third Stage: The third staging is the final stage of frozen shoulder. It is normally referred to as the Thawing stage. As the name suggests, in this stage the frozen shoulder begins to thaw, and the movement gradually starts to get enabled. At the end of this stage, the person can feel painless, and the full range of movement is enabled. The pain throughout these phases can usually be more severe during the night, which can severely impact the sleep of the patient causing restlessness.
Causes of Frozen Shoulder
The physiological cause of frozen shoulder includes the tightening and thickening of the ligaments, tendons and the connective tissues of the shoulder. The shoulder joint is very sophisticatedly covered by a combination of ligaments, tendons, and muscles, some of which serves the connective purposes. The inflammation and stiffness of these tissues can result in an inability of movement and pain. The exact underlying cause of this stiffness is still unknown to the researchers and doctors. However, certain risk factors are associated with this condition, such as an underlying health condition of a patient, including diabetes or a fracture. Usually, the primary cause of frozen shoulder is considered to be immobilization of the frozen shoulder.
Risk factors for Frozen Shoulder
There are various risk factors involved in the development of a frozen shoulder. Although it doesn’t mean that all such people will definitely develop the condition, these factors can significantly increase the underlying risk. Some of the most common factors include:
Age
Older people and athletes are more at risk of developing a frozen shoulder. People above forty years of age have a significant risk. Therefore, exercising is especially recommended.
Sex
Women athletes are more at risk of developing a frozen shoulder.
Lack of mobility
Partial lack or complete absence of mobility and movement of the shoulder can significantly increase the risk of frozen shoulder. This will include people who are required to limit their daily mobilization and exercise due to their lifestyle. A number of other factors can also influence the possibility of developing a frozen shoulder, such as:
- Fracture
- Health conditions like diabetes and Stroke
- Post-surgical complications.
- Rotator cuff injury
- Systemic diseases
- Hyperthyroidism
- Heart-related diseases
- Inactive thyroid
- Parkinson’s disease and neuropathy
- Tuberculosis
Prevention for Frozen Shoulder
Prevention is essential for minimizing the risk of frozen shoulder, especially in cases where patients have certain underlying health conditions. These preventive measures should include:
- Increased mobility of the shoulder
- Exercising and stretching
- Physical therapy in case of fractures
- Correct exercising in case of underlying diseases
- Lifestyle changes.
Exercising can significantly help in the reduction and the prevention of frozen shoulder symptoms. These exercises need to be simple if you have experienced recent trauma. However, they can very effectively decrease the risk and possibility of a frozen shoulder. Exercises like crossover stretching of the arm and others can help keep the tissues healthy and moving. Here we discuss some of the most effective exercises that can prevent frozen shoulder. However, it’s important to note that these exercises should be administered under the supervision or with the guidance of a specialist of a physical therapist.
Crossover arm stretch:
Stretching out the frozen arm to the front and pulling it to hold next to your chin for half a minute before releasing.
Pendulum stretching:
Hang your pained arm and swing it in a circular motion, gradually increasing the diameter of the circle with time.
Towel stretching:
With the help of a towel, pull the towel with the healthy arm from behind your back while holding it with both hands in order to move the pained arm up in the direction of the shoulder.
Diagnosis of Frozen Shoulder
The primary diagnosis is initially performed. In this diagnosis, only the medical history and the physical symptoms are evaluated carefully, such as apparent symptoms of pain and swelling. The doctor may also carefully examine by moving the shoulder joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists for the structural problems. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition.
Treatment of Frozen shoulder
The treatment for the problem of frozen shoulder can be multidimensional. Frozen shoulder is a more dynamic problem compared to other shoulder injuries. Therefore, the treatment approach may also differ depending on the type of condition and severity. Unlike other injuries, the problem of frozen shoulder can be very persistent, and the symptoms can remain for as long as three years. This deteriorates a quality of a significant portion of your life. Hence it is extremely important to take proper measures for the treatment of Frozen shoulder. All the treatments are aimed at alleviating the pain and improving the mobility of the arm by reducing stiffness. This can be done in a number of ways and with a combination of different treatment methods, such as injectable, medication, physical therapy and exercise.
The approach follows the following pattern:
- physical therapy
- medication
- surgery
- home care
Physical therapy is almost essential for all cases of the frozen shoulder due to the nature of the problem. The objective remains to be free movement of the shoulder joint without pain, which is where physical therapy plays an important role to stretch your shoulder joint and regain the lost motion. The recovery period can take anywhere from a few weeks to nine months to experience significant progress. If physical therapy is not leading to good results, in the long run, it is a very strong reason to see your doctor regarding the condition. Certain medicines can also be taken for relieving the pain as well as lowering the inflammatory condition that the shoulder may be suffering from internally or externally. The most commonly used drugs for this purpose is naproxen sodium, aspirin, and ibuprofen. In severe cases, you may be required to take steroid injectables. However, there are several side effects of steroids, and they should only be administered if there are no other options or any options except a surgery.
You should also take proper care at home and incorporate these changes and preventive measures in your everyday activities. This would include a regular administration of icing, compression, and other exercises. You also need to cut down on your everyday activities and limit the movement by bringing drastic changes to your lifestyle. An expert will be able to guide you on how easily and effectively you can carry out everyday tasks without the use or with minimal uses of your arm and the shoulder. Another treatment that can be applied for alleviating the pain is a hot and cold treatment which utilizes the difference between temperature extremes can also help alleviate the symptoms this is usually done by the padding or hot and cold packs that are available in the market. Your doctor will also guide you regarding the exercises that you should do and the exercises that you should avoid on a daily basis.
In case if other treatments are not showing positive results in the long run, you may have to opt for a surgical procedure. The procedure is invasive, but it may be inevitable in certain cases since we have talked about how persistent a problem of frozen shoulder can be. The stiffens and freezing may be a result of dislocation or a certain type of adhesion which is causing a jam. The surgery is aimed at removing the cause of the frozen shoulder after figuring out what the problem is after careful diagnosis. For movement of the arm and shoulder, joint anesthesia may be administered. Diagnosis, as well as treatment, may be carried out with the help of an arthroscope and arthroscopic surgical treatment. When the cause of frozen shoulder is an injury, you should look forward to performing surgery after a few weeks if no positive results of physical therapy are seen. After the surgery, your stitches will be removed in ten days. The rehabilitation and postoperative care, exercise, and physical therapy is the most important part to ensure that you get back to the ground at the earliest. Most athletes are able to continue with their sports within three months from the time of injury if effective treatment is given. Nonetheless, there are certain risks associated with the surgical procedures, and you should take some time out to discuss it with your doctor in detail and to think about it before getting into the treatment. Sometimes even surgery can be ineffective, and the pain may persist for a longer time.
Shoulder manipulation
The patient, in this case, is administered with anesthesia so that the pain cannot be felt. Under the impact of anesthesia, the specialist may move the shoulder joint to fix the dislocation that can alleviate the symptoms. This strongly depends on the type of the condition the patient is experiencing.
Transcutaneous electrical nerve stimulation
This is achieved by using equipment which aims at numbing the nerves that work as pain receptors. These nerves are numbed from the back and spine area. This method is also referred to as TENS, and it can be used to alleviate pain. However, this should only be administered by a specialist.
Sometimes surgery may be the only viable option in case of frozen shoulder, and to ensure faster results it is also often recommended. Here are some of the best measures that can be taken for the treatment of frozen shoulder:
- Resting as much as possible
- Icing the painting area
- Using compression bandages
- Anti-inflammatory medication
- Exercising, stretching, friendly workouts
- Gradually start physical activities, don’t rush.
- Surgery as a last resort, if no results and symptoms persist after the treatment.
Iliopsoas Syndrome
What is Iliopsoas Syndrome?
Iliopsoas syndrome is another name for iliopsoas tendonitis, which is a common condition in sports injuries characterized by the inflammation of the tendons or the proximal tissues or the area close to the tendons. It can be a result of overuse, overexertion, and repeated flexion of the hip muscle resulting in pain and inflammation caused by acute trauma. This is specific to the tendons of the hips. Although there are a number of other conditions that can affect the hip region, iliopsoas syndrome is one of the most common among the sports people and the athletes. This syndrome may cause tendinitis as well as bursitis of the hip. The iliopsoas is a regional muscle in the anterior hip, consisting of three main parts. These are named as psoas major, psoas minor, and the iliacus. These muscles serve the purpose of flexion of the hip. Bursae are also present in the hip joint similar to many other parts of the body. Bursa is the small sacs that are filled with fluids, and they act as the cushions to the bones, tendons, ligaments and the muscles in the proximal locations of the joints. In the hip, there are two bursae which are usually prone to inflammation. In simple terms, when one of these bursae becomes inflamed, the condition is known as hip bursitis, and when the tendons of iliopsoas which joints the thigh bone with the muscles are inflamed, the condition is termed as tendinitis.
Causes for Iliopsoas Syndrome
There are a number of different causes of Iliopsoas syndrome. Specific to the people involved in sports activities, Iliopsoas syndrome can be experienced most commonly due to the overuse and repeated use of a certain area. As most sports require repetitive movement of a certain part of the body, the athletes and sportsmen can become vulnerable to such conditions.
Other causes of Iliopsoas syndrome may include:
- Sudden jerking
- Running several steps
- Suddenly stopping while running
- Legs or arms stretching
- Wrong posture and legs movement
- Heavy hit
- Hard blows
- The weakness of the tendons
- Lack of flexibility of the tendons and muscles
- Tearing of the muscles
- Overexertion of joints
- Not stretching or warming up before working out
- Arthritis
- Length difference of legs
- Rheumatic arthritis
- Reactions of medication
- Abnormal placement or displacement of joints and bones
Symptoms of Iliopsoas Syndrome
Pain is the most important symptom of iliopsoas bursitis and iliopsoas tendinitis which can be aggravated by the movement. The pain can either be chronic or develop gradually over a long term, or it can be due to a sudden injury or blow in most cases. Difficulty or complete loss of movement ability is also experienced by the people suffering from iliopsoas bursitis and iliopsoas tendinitis. Occasionally the patient may also experience swelling, redness, and warming of the injured area. The symptoms you should generally look for are the following:
- Feeling pain and stiffness in the hip area
- Increased pain occurring due to movement or compression
- Redness and swelling.
- Difficulty or inability of moving hip due to pain
- Sharp and intense pain in the start
- Gradual dulling of the pain
- Clicking or snapping of the hip
- Increased Pain due to mobility
- Bruising and rashes
- Sharp and stinging pain during exercising
- Tenderness in the hip or groin
- Pain in the lower back
- Pain in buttocks
- Pain radiating along the leg
- Groin and pelvic pain
- Shuffling and limping
- Difficulty in maintaining an erect posture
Risk factors for Iliopsoas Syndrome
Age is not the important risk factors of iliopsoas bursitis and iliopsoas tendinitis. Apart from that the type of sports and the strength of tendons and muscles also have a significant amount of determining the impact on the risk of iliopsoas bursitis and iliopsoas tendinitis. Sex is also a significant risk factor, and females are more prone to iliopsoas bursitis and iliopsoas tendinitis. There may be several other risk factors involved in iliopsoas bursitis and iliopsoas tendinitis, such as:
- Overuse and overexertion
- Bone spurs
- Type of sports: Runners, athletes, dancers, soccer players
- Calcium deposition
- Previous injury or trauma of the hip
- Underlying issues related to hip and spine, such as arthritis and scoliosis.
- different types of arthritis
- The difference in the lengths of the legs
Diagnosis of Iliopsoas Syndrome
The diagnosis for iliopsoas bursitis and iliopsoas tendinitis can be a thorough procedure in certain cases. The patient is also mostly able to tell if the pain is muscular or if it’s in the bone. Nonetheless, the primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain, the inability of movement, bone condition, and swelling. Medical history also plays an important role here. The doctor may also carefully examine by moving the leg, hip and the joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an X-ray diagnostic test to identify the bone condition, an ultrasound test or an MRI (magnetic resonance imaging) test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound can sometimes help the doctor to locate and study the internal structures to see any possible damage.
Treatment for iliopsoas bursitis and iliopsoas tendinitis
The treatment for iliopsoas bursitis and iliopsoas tendinitis is rather simple in most cases as the condition is commonly not very severe. Surgery is avoided unless absolutely necessary, and the resting is considered to be an effective treatment method. The patient can recover from iliopsoas bursitis and iliopsoas tendinitis within a month only by resting. However, there are certainly several other things that you can do to ensure effective and speedy treatment and recovery.
The cause, as well as the severity of the condition, is very important for the treatment of iliopsoas bursitis and tendinitis. If the condition is mild, you can take proper rest and keep your joints relaxed. Several home remedies and traditional methods can be very effective, and in most cases, you may not need to see a doctor. The inflammation can be reduced by taking anti-inflammatory drugs and icing the swollen area to alleviate the symptoms of pain and swelling. Similarly, you need to bring some changes to your daily routine and the types of the activities that you’re involved in. This can effectively reduce the irritation caused to bursitis. Furthermore, you can make sure of aids like crutches and a cane to support yourself rather than putting your body weight and the pressure on your injured area. This will not only be protective, but it will also speed up the recovery from the pain and other symptoms. For complementing the treatment for effective results, you can try other available options such as medicines that are aimed at reducing inflammation. This can be more beneficial than taking the simple painkillers. Other than this, you may go for other NSAIDs and over the counter drugs, like acetaminophen and aspirins. In severe cases, if the condition is not tolerable, you can administer corticosteroid injections with the prescription of your doctor. Combining more than one treatment options can improve the effectiveness of the treatment overall. In terms of physical therapy, you should aim for strengthening and stretching exercises. These would be advised by your therapist depending on the types that are suitable for you. If you are practicing them on your own, you should discontinue them if it is enhancing the symptoms or cause more pain. The approach should be to stretch the hip flexor muscles. It is important to note that these conditions can be coupled with an infection as well. Therefore, you may need an antibiotic course after the diagnosis if your doctor finds a possible infection. Apart from that, surgery will not be required in a majority of cases. Some simple and effective measures for the treatment of iliopsoas bursitis and iliopsoas tendinitis are:
- Resting as much as possible
- Icing the painting area
- Anti-inflammatory medication
- Exercising, stretching, friendly workouts
- Physical Therapy
- Gradually start physical activities.
- Surgery as a last resort, if no results and symptoms persist after the treatment.
When the signs start showing improvement, the patient can gradually get back to carrying out their everyday activities that require physical exertion. The specialist or doctor will make sure of when you are in a condition to get back to continue with everyday activities. The patient should phase into the regular lifestyle by first of all trying light exercises and gradually improving on the difficulty. At the same time, you should ensure that you do not do anything that can cause jerking of the hip. It is best to avoid sports for a while after the injury. Sports should be avoided for a long time after the injury, even when the patient recovers, as it can severely increase the risk of reversing the healing.
Impingement Syndrome
What is Impingement Syndrome?
Impingement syndrome is a condition of the shoulder common in sports injuries that are characterized by pain inability of movement, weakness and limited mobility of the shoulder. There are several medical names for this condition, such as supraspinatus syndrome, painful arc syndrome and sub-acromial impingement. In more common terms it is also referred to as thrower’s shoulder and swimmer’s shoulder, given its strong association with these sports. The impingement syndrome is a result of irritation of rotator cuff muscle and the inflammation of proximal tendons.
Causes of Impingement Syndrome
The patient’s condition in Shoulder impingement is caused due to overuse, the repetition of the movement of shoulders and raising and stretching the arm due to which the tendons can impinge. That is why the condition is also referred to as rotator cuff impingement; these movements can include overhead movement, overuse of the joint and other similar activities. People involved in a variety of sports are vulnerable to this condition. Shoulder impingements may be very painful accompanied by the disability to continue sports for a while. The condition makes it very difficult for the patient to sleep, and they may get up from sleep several times during the night due to the shoulder pain. It’s also difficult to get a comfortable lying position where the shoulder doesn’t pain. The pain can get worse with moving the shoulder joint in certain angles, and it can be extended towards the rest of the arm. It can also make the usual everyday activities a challenge for the patient due to the pain, such as combing the hair.
Shoulder impingement affects the area where the upper arm is connected strongly in the socket, and this connection is strengthened by the group of tendons and muscles called the rotator cuff. Injury to this group of muscles can result in a dull pain in the shoulder. And the condition can easily get exacerbated while making the pain worse with time. Therefore, proper care, especially with the right sleeping position, is required to treat the condition in a timely manner and not cause further damage.
Signs and symptoms of Impingement Syndrome
The symptoms of the frozen shoulder may vary from patient to patient depending on the severity of the condition and the time period for which the problem has existed. The symptoms start to build up gradually, and the problem can span for a while. Pain, weakness, stiffness, and lack of mobility are the most important symptom of shoulder impingement which can be aggravated by the movement. The pain can either be chronic or develop gradually over a long term, or it can be due to a sudden injury or blow. Difficulty or complete loss of movement ability is also experienced by the people suffering from shoulder impingement. One such condition is known as adhesive capsulitis when it happens to the shoulder. This condition is separately characterized as the frozen shoulder. As a result, the shoulder gets frozen and cannot be moved. Occasionally the patient may also experience swelling, redness, and warming of the injured area. The symptoms you should generally look for are the following:
- Feeling pain and stiffness
- Increased pain with overhead movement
- Increased pain occurring due to movement or compression
- The feeling of grinding upon movement
- Difficulty or inability of moving joint due to pain
- Popping sensation upon movement
- Sharp and stinging pain during exercising
Risk factors for Impingement Syndrome
As a general rule, the overall resilience and strength of the patient is a very detrimental factor. If the muscles are wrong, the injury is likely to be less severe. Apart from that, the strength of the muscles can also be affected by growing age, especially after the age of forty years. Therefore, age is another important risk factor. The type of sports that a person is involved in is also detrimental to the risk. Sports like tennis, swimming, baseball, soccer, and golf are the high-risk sports. The professional practices, as well as the medical history of the patient and his family, is also very detrimental.
Diagnosis of Impingement Syndrome
Initially, the patient is examined for certain physical symptoms of pain, weakness, and stiffness. A medical history of the patient is also helpful in the examination and diagnosis. The doctor may also carefully examine by moving the shoulder joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound will help the doctor to locate and study the internal structures to see any possible damage.
Once the doubt is established, the doctor may administer different tests for verifying the impingement syndrome. These tests include the Hawkins-Kennedy Test, and the impingement test, in which lidocaine is injected to notice the improvement in the symptoms of pain and movement. If there are positive signs, the condition is considered to be an impingement syndrome.
Treatment for Impingement Syndrome
A multi-disciplinary treatment can be administered for impingement syndrome. Since the nature of the condition is inflammatory, a number of oral anti-inflammatory medicines can be used for effective reduction of the symptoms. The drugs that are most commonly used for impingement syndrome are ibuprofen, aspirin, and naproxen. There are potential side effects of these medicines as they are administered for a long period of up to 2 months on a daily basis. Impingement syndrome can be persistent in certain cases, and it can take a lot of time to recover from it even by effective treatment methods fully. These medicines may include some over the counter drugs. However, you should not use any of these on a long-term basis without the prescription of a doctor and without careful supervision of a specialist. The side effects may vary from person to person, and if the side effects are enhanced too much, you may have to stop the medicines. The most common side effects of these medications are bleeding and stomach problems. These medicines are given to target and treat the symptoms that are expressed in impingement syndrome, and there are no preferred or specialized medicines for this problem. The effectiveness of these medicines may also differ in each person. Therefore, a number of different medicines may be used one after another after a gap of 12 to 15 hours depending on the response of each medicine. If one medication does not show any results for you, the doctor may go for the other medicine. This is continued until the results are noticeable.
If these medications and drugs do not show any significant improvement in the condition, then your doctor may go for cortisone based injectables as a secondary treatment option. Cortisone is a substance that has effective anti-inflammatory properties, and it can show results quicker. The reason it is used as a secondary treatment option is that it can cause weakness of the tendons and the muscles as a side effect if it is frequently used. Therefore, it is used only when it is absolutely necessary.
Apart from medicines, the treatment of impingement syndrome may also involve exercises and physical therapy on a regular and daily basis. The most important exercises include stretching. Warm showers are also useful as you may be able to move the stiff and painful joint during a shower. Along with light exercises, you should also ensure that you do not participate in the activities that involve repetitive movement and exertion of your arm. Above activities should be especially avoided in this regard. The best exercising practices will be guided and introduced to you by your physical therapist. The physical therapy will be aimed at stretching and strengthening of the muscles through exercises.
If the condition is not improving with these measures, the doctor may go for another diagnosis and carry out some tests, such as arthrogram, Ultrasound, and MRI as differential tests. It will help the specialist understand if there is a need for surgery, or if there has been severe tearing.
In most cases, the patients are able to recover from impingement syndrome with the help of exercises, physical treatment, and therapy, therapeutic approaches, preventive measures, and injectables. It is important to ensure that the injured area should be given enough time to rest so that inflammation can be capped.
Treating the impingement syndrome with the therapeutic approaches, however, poses a number of side effects that you must be aware of. The patient may suffer from digestion problems, headaches, nausea, and stomach related problems. A useful measure would be to take your medicines after the meals to avoid severe side effects. Apart from these side effects, a person may also suffer from ulcers, bleeding, and constipation. However, these are the less common side effects. You can also adapt to an anti-inflammatory lifestyle and eat the foods that encourage the healing process. One of the highlight substance that you can use in your foods is turmeric or curcumin.
In case of a surgical procedure, you may go through a process of shoulder manipulation under the effect of anesthesia. If the shoulder is dislocated due to acute trauma, it will be fixed to relief the muscles and tendons that are stretching because of it. The damaged tissue or any adhesive particles are removed from the shoulder joint with the help of tube insertion. Physically, you can also administer the heat and cooling procedure which can help reduce the inflammation, swelling, and pain. A gentle massage can also be helpful in some cases if the area is not sensitive to touch. The improved circulation and blood flow due to the massage will help reduce the inflammation and enhance the healing.
Iliotibial band syndrome
What is Iliotibial band syndrome?
Iliotibial band syndrome (ITBS or IT band syndrome) is an overuse injury of the connective tissues that are located on the lateral or outer part of thigh and knee. It causes pain and tenderness in those areas, especially just above the knee joint.
Iliotibial Band Syndrome is a common medical condition in sports people and athletes that is characterized by an overuse injury of the Iliotibial Band. It happens due to the rubbing and the friction of the muscles against the knee bone. The Iliotibial Band is also referred to as IT Band, and this condition is also abbreviated as ITBS in medical terms. The Iliotibial Band is located in the outer and lateral region of the thigh, and it extends to the knee. This is basically a band of soft and firm connective tissues. The condition can cause mild to severe pain along with other symptoms like tenderness above the knee. The Iliotibial Band is stretched from the pelvis, crawls through the hip region and extends towards the knee. It mainly serves the purpose of keeping the knee stabilized when a person is walking, moving, running, stretching and exercising.
Signs and symptoms of Iliotibial band syndrome
The symptoms and signs for IT Band Syndrome can vary from person to person depending on the severity of the condition. In less severe cases the patient may experience a sudden discomfort just above the knee during a walk or run. The pain may go once the patient rests for a short while. For some people, the pain is not experienced suddenly and may build up gradually with time. In most cases, IT Band Syndrome cases include a stinging sensation in the knee along with the loss of control over the knee muscle, which may destabilize the knee. In severe cases, the movement of the knee joint is severely limited due to the pain, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling. Some of the other most common symptoms can include:
- Thickening of the tissue in the proximal region
- Burning sensation
- Increased pain with the passage of time
- Pain due to the striking of the foot on the ground
- Persisting pain in the IT Band
- Pain in the tibia upon compression
Causes of Iliotibial band syndrome
The most common cause of an IT Band Syndrome is the turning and the wrong training habits, imbalance of the muscles, and sudden displacement. As a result, the knee can be pushed out of its normal and natural position, and it can cause muscular and tendon damage. Such unexpected movements are very common in sports that involve a lot of running and the use of legs. These tearing of the muscles can be very painful at times and could be accompanied with other symptoms such as bruising and the swelling of the area. Although it’s mostly the tendons, ligaments, and muscles that are damaged or injured due to IT Band Syndrome, it can also damage other structures, such as the blood vessels, the knee by displacing it, and cartilages. There are several risk factors involved, such as the types of sports, etc. however, it can occur in people of all ages.
Some of the other most common causes for IT Band Syndrome include:
- Walking on uneven or hard surfaces
- Wearing the wrong sized or kind of shoes
- Rigorous sports activities and feet movements
- Twisting of feet, ankle and knee muscles
- Turning suddenly during a play
- A sudden strain due to kicking
- Running and stopping suddenly
- Continuing sports after mild strains and pain.
- Microtraumas
- Wrong diagnosis of a previously occurring pain.
- Repeated minor injuries
- Overuse of the muscles
- Long training hours
- Sitting in the lotus position for long hours
- Prolonged running on an uneven surface
- Uphill and downhill running
- Climbing and descending stairs again and again
- Not stretching and warming up before workout and running
- Hiking for long hours
- The weakness of abductor’s muscles and other tendons
Treatment & Rehabilitation for Iliotibial band syndrome
There are several ways to treat the IT Band Syndrome. The treatment may vary depending on the severity of the injury and the type of the underlying cause of ITBS. In terms of physical treatment, the traditional RICE therapy is widely used for IT Band Syndrome treatment. As a secondary relief, a number of painkillers and anti-inflammatory drugs can be used, such as naproxen, ibuprofen, and aspirins. The medicines should be carefully administered as it can interfere with other prescriptions for underlying health conditions. The main approach often remains to be 1) complete rest and 2) foam roller massage.
Physical therapy and home remedies have a number of ranked approaches, including stretching exercises, massages and foam roll. It can improve the injury condition and reduce the symptoms of pain and swelling. Usually, you do not need to visit a doctor. However, you may consider seeing a physical therapist if the symptoms are not being addressed by the home remedies. The physical therapist will focus on stretching and stretching exercises to improve the flexibility and reduce the friction between the rubbing structures in case of IT band Syndrome. The inflammation scarring and breaking down of structures is caused due to this increased friction.
A number of other options are also available, such as therapeutic ultrasound techniques, such as phonophoresis, which can reduce the irritation and soothe the softer tissues around the knee. Medicine is administered through the skin to reach the inflamed tissues directly. Sometimes electricity can be used instead of the medicine in this treatment, which is commonly known as iontophoresis.
A physical therapist would require to measure some parameters to ensure a good exercise regimen for you, including your ability to balance, your flexibility and the analysis of your gait. Certain aids and footwear accessories may also be used to reduce the problems associated with position and posture.
In case if the anti-inflammatory medicines are not showing positive results, the doctor may also have administered corticosteroid medicines on you which are directly delivered to the inflamed area with the help of injections. This can show a quick and effective response, but there are several side effects associated with it.
Surgery is rarely required for the problems associated with IT band syndrome. However, if an operative procedure is required, the doctor may administer an arthroscopic procedure to diagnose the condition of the inflammation and the scarring. This can be subsequently treated with the same procedure. The inflamed structure of IT Band is removed through the surgery. Apart from arthroscopy, the doctor may also operate to cut a triangular part from the IT band which will help to increase the length of the band. Surgery requires a rigorous examination of pre-surgical considerations that may be associated with the pain to ensure zero mistakes.
Biomechanical analysis
Identifying the cause is also an effective way to pursue treatment. A specialist or an expert, such as a podiatrist can help in to identify any foot or underlying muscular problem that is causing muscular stress and rotation.
Foam Roller
A foam roller can help massage and stretch the IT Band muscles while removing any ties and knots of the tendons. It can also help reduce the friction and massage the impacted area. It should be continued even after the pain is gone.
Overtraining Syndrome in Athletes
What is Overtraining Syndrome?
Overtraining Syndrome is a common medical condition experienced by people who are involved in sports and athletics. As the name suggests, Overtraining Syndrome is developed as a result of excessive training for a prolonged time more than the threshold capacity of the body. As a result, the athlete’s body undergoes serious damage in a number of ways. This usually happens to sports people when they do overstrain before a big competition or an occasion. Instead of benefiting from putting so much effort into it, the health and wellbeing are usually reversed, and it may take some time for the patient to recover from the damage caused due to Overtraining. This is also very common in sports people and gymnasts and usually happens when people overestimate their body’s potential and end up training themselves to the point of damaging consequences. Sometimes the symptoms of Overtraining Syndrome may also appear due to an inadequate amount of rest and not let your body recover from the previous workout. Technically, our body does not grow and become strong after a workout. In fact, our body grows strong after we have completely rested and recovered from our last workout. Rest is the point in time where our body grows and become stronger. Therefore, it’s essentially important that proper gap must be maintained between two consecutive workout sessions and enough rest and sleep is received. Otherwise, the results can reduce the performance, end up with pain, weakness and backfire the entire motive of the athlete. It may also take place due to overloading. It’s important here to maintain the right balance between resting, recovery, and overloading. The consequences will not only reduce strength but also cause pain.
Signs and Symptoms of Overtraining Syndrome
There can be a number of different symptoms associated with Overtraining Syndrome and may vary from person to person depending on the severity of the condition and the strength of the athlete or sports person before the Overtraining Syndrome. Pain is the most important symptom of Overtraining Syndrome which can be aggravated by the movement. The pain can either be chronic or develop gradually over a long term, or it can be due to a sudden injury or blow in most cases. Difficulty or complete loss of movement ability is also experienced by the people suffering from Overtraining Syndrome. Occasionally the patient may also experience swelling, redness, and warming of the injured area. A range of symptoms may be experienced based on the severity in terms of physical, mental as well as emotional symptoms. It greatly depends on the person suffering from it. However. Here are some of the most common symptoms that are experienced by people suffering from Overtraining Syndrome:
- Lethargy and exhaustion
- Lack of vitality and energy
- The feeling of being washed-out
- Pain in any part of the body
- Specific pains in joints and muscles
- Stiffness in the impacted region
- Difficulty in movement
- Lack of willingness to do little things
- Drastic reduction in performance
- Soreness in the legs
- General Pain in different body parts
- Persistent headaches
- Difficulty in falling asleep
- Restlessness
- Weakened immune system resulting in infections
- Depression and anxiety
- Becoming prone to injuries
- Irritability and mood swings
- Reduction in stamina
- Lack of interest and enthusiasm
- Not feeling hungry at times
This condition of Overtraining Syndrome is comparatively different from other sports injuries, as it impacts the body in various ways, including emotional, mental and physical symptoms. Most of the body’s energy starts being utilized in the recovery of the patient which can impact the efficiency of other functions and body processes.
Diagnosis of Overtraining Syndrome
The diagnosis of overtraining can be relatively different from other injuries caused due to sports activities. Usually, the symptoms are quite clear to the patient. The first stage of diagnosis could be a physical examination and the symptoms that the patient is suffering from. It can take it easier to diagnose the exact underlying cause behind the overtraining syndrome. There are a number of different ways through which you can identify and objectively measure the possibility of overtraining syndrome. Firstly, if there are people around you who are noticing that you’re working too hard on yourself, they’re most probably right. So, don’t ignore such comments if they’re coming from genuine people. One telling method for testing this syndrome is to measure the rate of your heart over the span of equal intervals. The measure for the speed as well as the aerobic heart rate can be measured and noted down. If you experience a lack of stamina along which increased heart rate at rest, there is a significant possibility of overtraining syndrome. The heart rate can be measured in the morning as well, which will show an increased figure if the problem persists. Another test for the condition is known as orthostatic heart rate test which can help in determining the overtraining syndrome. This test includes a number of steps, which are:
- Laying down and relaxing for ten minutes in the morning preferably
- Note down your heart rate right after that
- Stand up for fifteen seconds and then take another record for heart rate. Then take another after 90 seconds, and the fourth one after two minutes.
People who are suffering or about to suffer from overtraining syndrome will show a striking increment of ten beats per minute on the fourth measure compared to the first one, unlike the normal athletes that don’t experience any significant change. This can indicate that the patient is or is about to suffer from overtraining syndrome, is exhausted, experiencing fatigue and he’s not resting properly. This test along with the other measured trends can give a good idea about the condition of the patient.
Psychological tests are also known to be the most effective methods for understanding and diagnosing the overtraining syndrome. As we discussed before, the overtraining syndrome can also have emotional and mental consequences, which can give a good measure of the condition. Usually, the patient may experience reduced mental capability and confused mental state. The patient may also experience emotional trauma, depression, anxiety, unenthusiastic thoughts, negative feelings, mental fatigue, irritability and anger, and other such symptoms.
Treatment for overtraining syndrome
There can be a number of different ways in which you can alleviate the symptoms of overtraining syndrome. It Although it’s not an extremely dangerous condition, it is a very common problem, and you may want to take medication if you need assistance. Depending on the severity of the condition you and your doctor can choose the right treatment option for you. Since it is a common problem, you can solve it by using a number of different self-treatment options. Some of the most effective approaches are as follows:
Complete Rest
The very reason for overtraining syndrome is not resting enough. Once you get it, you need to take complete rest for a while and pause your sports activities. The condition can develop over time, and it takes longer to treat a more prime condition. Therefore, you must actively monitor it for early detection. In mild cases, you only need to rest for 3 to 5 days. In moderate cases, you may rest a little longer than a weak. The best way to know if you have rested enough is to test for movement and pain.
Cross training
Even though resting the over-trained part is important, in mild cases, you can utilize that time to train other parts of your body in moderation. You do not have to train too much as you need to preserve some of your body’s energy to treat itself. This is a dangerous line because if you overstrain yet another area of your body you increase the risk of developing a secondary condition of parasympathetic (PSN) and sympathetic nervous system (SNS).
Utilize for spot train
While you are giving time to your over-trained area to recover, you can use that time to strengthen and train the weaker and undertrained areas. This is the time for practicing preventive measures and avoiding overtraining and other injuries in future.
Early treatment
You do not want to delay your treatment even for a day. Once the mild symptoms start to show you should immediately stop the workout and training and start your treatment. The more you ignore it, the more it will get persistent and difficult to treat.
Pain Management
You need to be active in terms of managing your pain. You don’t want to make it worse if you are continuing your daily activities. For that, you can use the foam roller as well as gentle massages from a specialist or physical therapist. They can also teach you how to massage the area yourself and how you can use the foam roller.
Acupuncture
Acupuncture is an old but gold therapy for the treatment of pains and inflammatory conditions. You can easily incorporate the acupuncture technique in your treatment plan. This is known to improve the conditions associated with different body structures such as the nerves, muscles, tendons and other structures.
Healthy diet
We are what we eat, and when we train to consume our muscles and body tissues, they need to grow again. Our food is what provides us nutrition, energy and the development of our muscles. By eating healthy we do not only wipe out the chances of damage, but we also provide the raw material for the rebuilding of our muscles after we have damaged them.
More water and supplements
Drinking more water will ensure proper detoxification of the muscles and improved nutrition and healing. You should also couple it with supplements that can boost up the healing power of your body. You can try supplements that include organic glucosamine and chondroitin. Apart from these, you can try a natural treatment that can reduce inflammation and boost up the healing capacity of our body, such as curcumin.
These factors will determine the type of pain the treatment method is chosen to be administered. The most common treatment methods that are used for overtraining syndrome including resting, keeping yourself hydrated at all times, getting a relaxing massage or a sports massage, and start with the cross training. Rest is certainly the most necessary and most effective treatment for this condition. You should also ensure that you relax physically, mentally and emotionally. Don’t hesitate to pamper yourself for a while and do what you feel like doing. Massages also work great in this condition. This can include sports massages as well as relaxing massages, as you are trying to allow your body to relax as much as possible and get into the resting phase. Massaging the sore muscles can also help a great deal. Also, eat foods that fight inflammation and have healing properties. Hot baths can also help you relax mentally, and alleviate the pain and soreness, so don’t hesitate to try a sauna. Massages, on the other hand, can increase the overall blood flow in the region and help speed up the recovery. Apart from this, you can also try cross-training as it can significantly help you relax physical and mental symptoms. Apart from these measures, you should also ensure that the exercises and physical activities are significantly minimized, and immunity building foods should be consumed. Nutrition also has a lot to do with the treatment of overtraining syndrome.
Prevention of Overtraining Syndrome
It’s easy to overestimate your body’s capabilities as we don’t feel the symptoms as long as our body is warm during the work out in most cases. However, the best way to go about with the preventive measures for overtraining is to make sure that you monitor and track your activities as well as training sessions to keep a bird’s eye view on what’s happening. Writing and noting it down can do more good that you think it can. Once you have your records, acting smart and increasing your workout regime gradually is the right approach. It’s difficult to precisely tell the exact measures and the time schedules since it has a broad scope and it’s different for each sportsman or athlete. Some people have more capacity than others. Keeping track of your activities will ensure that you don’t work more than you’re supposed to work each day, even when you feel like you’re perfectly fine and can take, let’s say another hour of rounds. Also keep a keen eye on the symptoms and the warning signs as discussed above, as it will help you understand if you’re at the verge of developing the overtraining syndrome, and help you protect yourself from it promptly. Keep a healthy nutrition regime and rest well on the rest days. Also, avoid monotonous training and keep yourself hydrated. Also stay away from stress and depression as it can have serious physical consequences. If you have a previous injury in the leg, save yourself from heavy training even for the arms, as your body’s entire energy is concentrated on recovering you from the injury of your leg, and overburdening your body with a heavy workout at that point can cause problems.
Overuse Syndrome
What is Overuse Syndrome?
Overuse syndrome is a very common medical condition in the sports injury regime. It is experienced by most people involved in sports that require repetitive and overuse of certain parts of the body. The term overuse syndrome can go synonymously with terms like repetitive strain injury or chronic injury. An easy way to understand this syndrome is to classify injuries in two types. The first one being acute injuries, which takes place suddenly due to an accident or a single, instantaneous trauma or an injury caused due to hitting or a heavy blow. The second type of injury could be an injury which chronically takes place by gradual micro traumas or symptoms building up over a period due to repetitive unnoticeable injuries. In the end, the impact and symptoms combine to develop a serious condition. Overuse syndrome can be considered as the second type of condition that we have just discussed. It can further be classified into different types, such as occupational overuse syndrome (OOS), or sports overuse syndrome. Here, we will specifically talk about the sports-related overuse syndrome.
Sports-related overuse syndromes can occur in a variety of ways, to some different locations and body parts, causing some different conditions, over some different time periods. This is because the overuse syndrome has such a broad scope. It can happen to your muscles, or to your bones, to your tendons, or to the ligaments and other tissues. The injury can cause damage to the blood vessels or put pressure on your nerves, and it can impact certain organs or other bodily structures. There is a variety of conditions, and consequently a variety of different symptoms. However, certain symptoms are characteristic to this condition and may be used to diagnose and identify overuse syndrome. This condition due to its various forms can be mistaken as other conditions, such as overtraining syndrome as previously discussed which has certain, but not all symptoms of this condition. In some cases, it can become an underlying cause of a completely different sport-related injury, such as runner’s knee, ankle strains, shoulder dislocation, Achilles tendinitis, jumper’s knee, wrist fractures, tennis elbow, golfer’s elbow, swimmer’s shoulder, shin splints, and hamstring muscle strains. Although it may sound like a rare condition, overuse syndrome is more common in sports-related people compared to acute injuries and sudden traumas.
These conditions can develop over a long period with mild or very subtle symptoms, which is why it’s normally ignored and left unnoticed. However, these micro symptoms can eventually build up into something more serious and dangerous. Just like the onset of this condition is slow, the offset and recover are also usually slow.
Causes of Overuse Syndrome
The human body is capable of enduring a lot of pressure despite being fragile. We often take it from granting the way it protects us every day from millions of germs trying to attack us. Similarly, we have a natural defense mechanism to endure physical stress. Just like germ attacks strengthen our immunity, physical stress can strengthen our body and physical features. However, when the germs are too much and more than the capacity of our body and immune system, we fell sick despite our defense system. Similarly, when we overuse a certain part of our body despite having a body’s natural endurance, we can get that part damaged. Additionally, if we keep increasing the pressure and stress gradually, the body will slowly get used to it, and eventually, the body becomes stronger than before.
That’s how this whole thing works, and it’s important for us to understand this process to avoid overdoing. So basically the primary cause of overuse syndrome is the overuse and repeated use of a particular muscle, bone or tendon. Our body gets stronger through a process is known as remodeling. This process includes both production and destruction of tissues in our body. Therefore, it needs time to occur. If the tissues are not given enough break time after the destruction of tissues to recover and make new tissues, and if we continue which the exercise at the same time, it will create a condition in which the breakdown or destruction process becomes faster than the healing and generation process. As a result, overuse syndrome is developed.
Risk Factors for Overuse INJURIES
There are some factors involved in the risk of overuse syndrome. These include the errors in the training practices and effectiveness of the exercise, the capacity of an individual and their behavior. Some of the most important risk factors are:
- lack of strength of the bones, tissues, ligaments, tendons, and muscles
- deficiency of vitamins, calcium and other minerals
- wrong practices and training effects
- repetitive and careless movement of a single area
- Higher frequency of repetition with shorter intervals.
- Older age
- The type of sports
- Continuing sports after a long break
- Enthusiastically overworking
- Pushing for forced performance
- Working beyond capacity intentionally or unintentionally
- improper technique
- lack of flexibility of different areas of the body
- alignment and balance issues in certain people
- the unsymmetrical and disproportionate body structure
- incomplete recovery from the previous injury
Diagnosis of Overuse Syndrome
Pain and swelling are the initial signs that are observed during the primary diagnosis. The overall condition of the injured area is also examined by the doctor carefully. The doctor may also carefully examine by moving the knee joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the Ultrasound will help the doctor to locate and study the internal structures to see any possible damage.
Treatment for Overuse Syndrome
There are some ways in which the underlying overuse syndrome can be treated. However, the treatment option is chosen after the diagnosis depending upon the location, type, condition, severity and several other factors. We have previously discussed in detail about numerous specific overuse injuries resulting from an overuse syndrome. Here are some general ways for going about the treatment of overuse syndrome.
- drastically reduce or change the workout, its frequency, and its intensity
- Practice cross-training to allow the recovery and relaxing time by alternating hard and easier workouts.
- Improve your technique and remove training errors.
- Try temperature changes, and heat and cooling treatment
- do stretching and warming up before sessions and workouts
- Use ICE as discussed in detail for the specific cases.
- OTC Drugs, painkillers and anti-inflammatory medications upon need.
- Physical Therapy
- Massages
- Acupuncture technique
- See a doctor is the conditions persist.
Preventive measures for Overuse Syndrome
Stretching of the muscles is a good way to stop and treat overuse syndrome. However, it’s not recommended in all situations. The stretching can be done by softly allowing the muscles to move and function in the proper way they’re meant to function. The prevention is usually more about common sense and some knowledge, and the patient can understand what is needed to be done with a little knowledge and interaction with the pain. Massage oil can be used for the prevention.
- Warming up and cooling down
- Keeping yourself hydrated at all times
- Avoid overexertion and fatigue
- Keep electrolytic balance
- Keep up with vitamins and minerals
- Take healthy nutrition
- Ensure proper intervals and rest time
Plantar fasciitis
What is Plantar Fasciitis?
Plantar fasciitis is a medical condition which is very common in people who are involved in sports and athletic activities. Plantar fasciitis is a condition that characterized by pain and inflammation in the fibrous tissue which is also known as plantar fascia. The fibrous tissue is located at the bottom side of your foot, and it helps to connect the heel bone of our feet to our toes. The condition can be in most cases severely painful and inflammatory. The pain caused due to plantar fasciitis can be very troubling, and it can also cause disturbances to our day to day life, resulting in problems with the exercise regime as well as sports training, also making it difficult for you to walk in certain cases. It may be due to inflammation of the muscles, ligaments, tendons, nerves, and tissues. Bearing any weight, even of your own can cause you problems and make the condition even worse. It can be a result of spraining and repetitive injury or trauma. The condition can also cause other characteristic symptoms, such as redness, stiffness, and swelling. The condition can also put pressure on the nerves that are located near the area. People involved in sports are the most vulnerable ones. However, other people may also experience plantar fasciitis.
Severe pain and stabbing pain can be experienced due to excessive and prolonged sitting, or early in the morning. It can also make it difficult to walk and to climb stairs. Usually resting is recommended along with other treatment options. Plantar fasciitis is the largest ligament in our body. It can be caused due to another underlying health condition in certain cases. The condition can also be mistaken with quite a similar condition called Baxter’s neuritis, which is due to nerve entrapment in the heel. If the condition remains persistent for more than a year, then it transforms into a more severe and chronic condition known as plantar fasciosis.
Causes for Plantar Fasciitis
There are some different causes of plantar fasciitis. The most important and common causes are indicated below:
- Too much tension and stress on the bowstring
- Tearing of the fascia
- Overuse injuries
- Repetitive trauma
- Microtrauma
- Irritation and inflammation
- Sudden jerking and a heavy blow
- Thin soled shoes or worn-out shoes
- Tightened Achilles tendons
- Being flat-footed
- Wrong walking and running positions and angles
Risk factors for Plantar Fasciitis
There are several risk factors involved with plantar fasciitis. Some of the most important ones are:
- Age. Plantar fasciitis is most common between the ages of 40 and 60.
- Wrong shoes: wearing the wrong sized shoes, too flat or high heels
- Types of sports: certain sports poses a greater risk of plantar fasciitis.
- Type of exercise: Certain exercises may cause too much pressure and stress on the heel area. Such as dancing, running, jumping, soccer and other similar sports.
- Foot types: Certain people have a flat-foot type, which increases the risk of getting plantar fasciitis problem. An arch is usually a good thing.
- Being overweight can also increase the risk of plantar fasciitis in most people as it increases the pressure and weight put on the heel.
- Standing for prolonged hours can significantly increase the risk of inflammation in the heels and cause a condition like plantar fasciitis.
Treatment for Plantar Fasciitis
Some different treatments can be administered to alleviate the symptoms and treat the condition of plantar fasciitis. The most effective ways to treat the condition includes.
Resting
Resting is the single most effective treatment for plantar fasciitis as it can allow your heel the time to recover from the underlying cause. Make sure that you rest your feet as much as possible, as a wrong pressure and movement can reverse the healing and make the condition worse. You should completely avoid walking around and bearing any weights for a while. Furthermore, icing can help alleviate the symptoms of pain and swelling, while speeding up the healing process at the same time. Plantar fasciitis is a common orthopedic condition of inflammation of feet, and the doctor may administer some different treatment options available for it.
Steroid injectables
The doctor may administer steroid drugs if the pain is not getting suppressed from the painkillers OTCs and NSAIDs. The substance is directly injected into the inflamed plantar fascia. This can effectively reduce the pain on a temporary basis for a month. Besides being a temporary solution, the treatment also has some different side effects.
Physical therapy
You may need physical therapy in case if the treatment with medicines, ice, and rest is not showing significant results. Your physical therapist will administer some designated treatment exercises. He will also guide you with the strengthening and stretching exercises of Achilles tendon, muscles of the lower leg and plantar fascia. He may also practice ultrasonography, contrast baths and massages to ensure better results.
Shock-wave therapy
As a name suggests, the therapy is administered to shock the plantar fascia area with the shock sound waves. It is done for simulation and enhancement of blood flow and circulation in the inflamed area. The waves can also reduce the pain as the nerves get stunned due to the shock caused by these waves. This literally “shocks” your plantar fascia with sound waves. It stimulates blood flow in the foot and helps the tissue heal. It also stuns your nerves to stop the pain.
Tenex procedure
It’s an operative procedure which involves cutting through a small area of skin. It’s a short procedure and only takes minutes to complete. The ultrasound technique is used through the cut area to remove the inflamed tissues. Upon successful completion of this treatment, the patient can get back to normal activities in a couple of weeks.
Icing
Icing can help alleviate the symptoms of pain and swelling while speeding up the healing process at the same time.
Anti-inflammatory foods and drugs
Also, eat foods that fight inflammation and have healing properties. Turmeric, also known as curcumin is also a magic ingredient which has amazing healing properties. Apart from that, you can use anti-inflammatory drugs which can alleviate the symptoms.
Devices
Certain aids and devices can be used for the treatment of plantar fasciitis when the conventional treatments are not giving any significant results. In the case of plantar fasciitis, devices like night splints, braces, crutches, and special footwear may be used.
Soft tissue Injuries
What is a Soft Tissue Injury?
We all are to experience injuries at some point in life. People who are involved in sports have a greater risk of getting several injuries during their career. While most injuries aren’t serious and easily treatable, certain injuries can cause serious and permanent damage. Depending on how delicate the injured area, muscles and tissues are, the lighter blow can have a greater impact. Sometimes little things that we hardly notice may end up developing a greater health condition. Soft tissues can be defined as the tissues that usually serve the purpose of the surrounding, supporting and connecting other tissues, organs, bones and structures inside our body. This group of soft tissues may include the nerves, tendons, muscles, fascia, and tendons. There may be other structures included in this group as well, such as blood vessels, fibrous tissues, synovial membranes and the fats. Wearing and tearing of soft tissues can be relatively easier and may cause severe problems. Sports injuries can easily cause damage to these soft tissues. Although some people may not consider it a remarkable problem, in most cases the OTC drugs and painkillers may not be sufficient to treat this problem.
Causes of Soft Tissue Injury?
A blow, hard hit or trauma to the tendons, ligaments, and muscles can cause soft tissue injuries. The condition is characterized by pain, swelling, and other similar symptoms. Soft tissue injuries can result from some different causes, including anything that can potentially damage the tendons, ligaments, muscles and other structures. It usually results in pain and can be accompanied by some different symptoms. Some of the most common causes of soft tissue injuries in the field of sports could be:
- Falling
- Bruising
- Heavy blow
- Bursitis
- Twisting of muscles
- Sudden trauma
- Tendonitis
- Sprains
- Strains
- Contusions
- Bruises (contusions)
- Stress injuries
- Leg displacement or foot displacement while running.
- Wrong posture and legs movement
- Sudden jerking
- Heavy hit
Signs and Symptoms of Soft Tissue Injury
Soft tissue injuries can cause acute symptoms. Pain is the most important symptom of Soft tissue injuries which can be aggravated by the movement. The pain can either be chronic or develop gradually over a long term, or it can be due to a sudden injury or blow in most cases. Difficulty or complete loss of movement ability is also experienced by the people suffering from Soft tissue injuries. Occasionally the patient may also experience swelling, redness, and warming of the injured area. The symptoms you should generally look for are the following:
- Feeling pain and stiffness
- Increased pain occurring due to movement or compression
- Difficulty or inability of moving in certain cases
- Sharp and intense pain in the start
- Gradual dulling of the pain
- Increased Pain due to mobility
- Bruising and rashes
- Sharp and stinging pain during exercising
- Tenderness
- Discomfort
- Redness
- Weakness
- Instability
- The inability of function due to severe tearing
The degrees of soft tissue injuries
There are different grades for soft tissue injuries such as strains and sprains, similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three grades are:
Degree 1
This is characterized by less than moderate pain, while the patient retains the ability to feel and move the injured area.
Degree 2
This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
Degree 3
This is characterized by severe pain, while the patient loses the ability to feel and move the injured area.
Treatment for Soft Tissue Injuries
There are several ways to treat the Soft Tissue Injuries. The treatment may vary depending on the severity of the injury and the type of the underlying cause of Soft Tissue Injuries.
Graston Technique
Graston technique breaks up the jam and adhesions which enhances the circulation and blood flow to the inflamed and injured plantar fascia. It involves special instruments that are used for a high-pressure therapy. It is used for the treatment of some other injuries, such as lumbar strain, carpal tunnel, and Achilles tendon apart from Plantar Fasciitis. It can improve the range of movement and reduce the symptoms.
Pain reduction
Severe pain is associated with soft tissues injuries in most cases. To reduce the symptoms and alleviate the pain, various approaches can be taken, such as over the counter drugs, painkillers, anti-inflammatory medicines, and other natural substances. The doctor may also use mechanical treatment options such as TENS machine for alleviating the pain.
Full Range Movement
Soft tissue injury treatment involves the recovery of the full range movement of the injured area. This is usually done by the administration of a complete physical therapy treatment plan. It includes a range of different exercises depending on the type of injury and the area that is damaged.
Proprioceptive Retraining
In cases of soft tissue injuries, the pathway of nerves can also get damaged which can result in severe pain. This can inhibit a person’s ability to move the injured area voluntarily. This condition is referred to as proprioception. Some different exercises may be practiced to recover this problem.
Heat or Ice
Heating the injured area can significantly reduce the symptoms of pain and improve the range of movement. It also enhances the blood flow and circulation in the injured area. Similarly, icing the injured area can alleviate swelling, inflammation, and pain. It should be administered repetitively for a few days to see results.
Following these treatments, a person should keep up with the rest and R.I.C.E protocol for the treatment of soft tissue injuries. Resting will ensure that the condition does not get worse and further injuries are prevented. Similarly, depending on the location of the injury, a person can use bandages and elastic bands under the supervision of an expert.
Active Release Techniques
Active Release Technique (ART) is a useful technique that can be implemented in case of overused muscles resulting in soft tissue injuries. It is beneficial both for the treatment of chronic as well as acute conditions. It can be used in case of muscle tearing, hypoxia condition, and other acute damages. An expert examines the condition with his hands and uses manual tension to stretch and lengthen the muscle. The specialist works when the muscles of the injured location are active.
Trigger Point Dry Needling
Dry needling technique is also useful in case of soft tissue injuries. It uses a sterile and ultra-sharp dry needle to alleviate the pain in the inflamed area. The technique is completely different from the conventional acupuncture. It utilizes the trigger points that are bands of muscles which are stimulated. As a result, pain and tension are reduced, and the circulation of the blood is increased in these areas. Acupuncture and massages can also be useful in alleviating the symptoms and reaching similar results.
Training Correction
Most of the soft tissue injuries are associated with wrong and improper training habits and practices. Your treatment plan should also include a proper corrective action plan regarding training. You may want to reduce or eliminate certain specific things that you do during your sports period. Your physical therapist can guide you by witnessing your practices to differentiate good practices from bad practices.
Medication
Some drugs can be effective in reducing the symptoms and alleviating the pain that is caused by it. You can use anti-inflammatory drugs, corticosteroid injectables, and cortisone injections. In mild cases, you should completely avoid heavy medication and stick to the usual over the counter medicines.
Soft Tissue Injuries are usually treated by non-surgical procedures unless the injury is extremely severe. Nonetheless, the treatment method depends on the severity, degree and the type of injury.
Preventive Measures for Soft Tissue Injury
There are some precautionary measures that you can take to prevent soft tissue injuries. Stretching of the muscles is a good way to stop and treat soft tissue injuries. However, it’s not recommended in all situations. In repeated injuries, the stretching can be done by softly allowing the muscles to move and function in the proper way they’re meant to function. That should be achieved through physical therapy. The prevention is usually more about common sense and some knowledge, and the patient can understand what is needed to be done with a little knowledge and interaction with the pain.
- Warming up and cooling down
- Wearing proper sports gears
- Properly using the equipment
- Taking rests and breaks frequently
- Gradually increasing the intensity of the workout
- Strengthening muscles and making them more flexible
- Communicate with your body and understand what it’s telling you
- Keeping yourself hydrated at all times
- Avoid overexertion and fatigue
- Keep electrolytic balance
- Keep up with vitamins and minerals
- Take healthy nutrition
- Ensure proper intervals and rest time
Dehydration
What is Dehydration?
Dehydration is a common medical condition that occurs in people associated with sports and athletics. It is a condition that is characterized by excessive loss of water content and the fluids from the body due to perspiration, heatstroke and other similar reasons. The condition may sound a mild one. However, in certain cases, it can be severe and extremely dangerous. Sometimes this condition can cause life-threatening symptoms, and it must be addressed on urgent bases. 70 percent of our body consists of water content. Similarly, each cell of our body also has a lot of water content. Dehydration can even remove water from our cells, causing them to dry out and die. It can also raise our body temperature to strike and shooting degrees which can be extremely dangerous. People involved in outdoor sports are at great risk of dehydration. During rigorous activities, our body burns a lot of energy, due to which excess heat is produced. As a result, perspiration works as a natural function of our body to remove the heat content along with the water and cool down our body. Too much perspiration can deprive us of the water content of our body, and that is what happens during the sports activities. Athletes and sportsmen can easily forget to keep up with their fluids intake, and they may need urgent medical attention. However, if action is taken promptly, it’s easy to alleviate the impact of dehydration by quickly increasing the fluid intake to cover the loss.
Symptoms of Dehydration
The most important symptom of dehydration in sports people can be thirst and vertigo. However, in some cases, the patient may not feel thirsty due to the thoughtful attention towards the play. The symptoms can be sudden and urgent action is required. The most common symptoms that are experienced by sports people and athletes during dehydration are:
- drying of the mouth
- Increased Thirst
- No thirst
- Lethargy and exhaustion
- Feeling dizzy
- darker urination
- feeling headaches
- reduced or no sweating
- The sinking of the eyes
- dry skin and shriveled skin
- Hypotension
- Faster heart rate
- Feeling feverish
- Increased body temperature without fever
- Hallucination
- Loss of consciousness
Causes of Dehydration
There are many different causes of dehydration, such as:
- Diarrhea
- Sweating
- Vomiting
- Diabetes
- Frequent urination
- Burns
Anything that causes the water to leave our body in excess quantities can cause dehydration. All these causes aren’t related to sports directly. However, they can be indirectly related. Nonetheless, the most relevant cause of dehydration in sports people is sweating and forgetting to drink enough water. Sometimes certain areas may not have access to drinking water such as in case of adventure sports, which is another reason for not drinking water leading to dehydration.
Risk factors for Dehydration
Several factors may increase the risk of dehydration in sports people, such as:
- Higher altitudes.
- endurance sports like marathons
- chronic illnesses
- Adrenal gland disorders.
- Age: more common in older people
- kidney disease
- cystic fibrosis
- Diabetes
- alcoholism
Complications of Dehydration
Dehydration can lead to certain complications resulting in secondary conditions, such as:
- It may result in seizures due to electrolyte imbalance
- Reduced volume of blood
- It can cause kidney related issues
- heat stroke
Diagnosis of Dehydration
The primary diagnosis includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The doctor may also carefully examine the medical history of the patient. A rational assessment and examination are also performed to see the characteristic symptoms. The mental examination aims to look for symptoms such as:
- Confusion
- Disorientation
- Irritability
- Physical Symptoms which are expected to be found include:
- Increased Heartbeat
- Hypotension
- Reduced sweating
- Reduced elasticity of the skin.
Once these tests are done, and the doubt is established, the doctor may test for dehydration. In most cases, the dehydration can be quickly recovered by giving fluids. Therefore, these tests may not be required. Nonetheless, the diagnostic tests for dehydration may include:
Blood tests
Several indicators are observed in the blood sample of the patient, such as electrolytic imbalance and the function of the kidney.
Urine Test
A urine test can tell if a person is suffering from dehydration.
Treatment of Dehydration
The single most important and effective treatment of dehydration is recovering the lost fluids and water content. Along with this purpose in mind, electrolyte recovery should also be kept as primary importance, since an electrolyte imbalance can result in serious consequences. The treatment for dehydration varies greatly with several factors, such as age, the reason and cause behind dehydration, the severity, and the type. However, those cases are not relevant to sports-related dehydration. For people involved in sports, the best way to recover from dehydration is cool water. Athletes should also always keep electrolytic drinks along with them all the time. Perspiration and sweating can also take away certain salts from our body that works as electrolytes. That’s why this approach remains to be very useful. Nonetheless, this isn’t a condition which can be taken lightly. The patient should at once be sent for emergency treatment. As small as it may sound, dehydration is a problem which is also capable of taking lives. In severe and urgent cases, the fluids and electrolytes are directly administered intravenously in the vein for quicker response.
Nosebleed
Nosebleeds are one of the most commonly occurring medical condition when it comes to sports and athletics. This can be a result of an injury in most cases. However, there can be other causes depending on the person who may vary from patient to patient. A sudden and acute injury or trauma, such as a heavy blow or a fracture of the nose can cause nose bleeding. Other minor injuries can also result in a nosebleed without much of an effort.
Symptoms of Nosebleed
Blood loss is the primary and characteristic symptoms of nosebleeds. Apart from that, the patient may or may not experience pain depending on the part injured and the severity of the condition. Sometimes it could be due to a heat stroke, a heat build-up or something similar. Blood can be lost from either of the nostrils, or it can also occur from both of them at the same time. Usually, the color of the blood is bright, indicating oxygenated blood. However, it is also likely to lose darker blood from the nose. The blood can run down and out from the nostrils, or it can go into the throat from the respiratory passage. Blood in the throat can also cause nausea and even vomiting to most people due to repulsive taste.
Causes of Nosebleed
Most of us have experienced or witnessed a nosebleed at some point in our life. Common sense correctly tells us that nosebleeds related to sports injuries would primarily be due to trauma, a high impact hit, a heavy blow, a fracture or any form of injury that may cause a rupture of the vessels carrying the blood or bleeding due to some other reason. These are the most common causes of bleeding from the nose in the sports niche. Certain health conditions can also cause bleeding from the nose. However, it’s less likely for the people involved in sports. These health conditions may include infection, fever, problems with heights, side effects of medication, sinusitis, cold, and diabetes.
Treatment for Nosebleed
Nosebleed in most cases is not a very serious or life-threatening condition unless the trauma has caused damage to the brain as well. The treatment is relatively simpler compared to other conditions. The type of treatment administered greatly depends on the diagnosis and the underlying cause of the nose bleeding. Therefore, in severe cases, a diagnosis becomes very important, and the patient should rush to the hospital or seek medical assistance at once. After the diagnosis, the doctor will assign to you an easy to follow the treatment plan that you can practice at home. The very first response should be immediate first-aid care to alleviate the symptoms and stopping the bleeding at once. All the athletes and sports people must be well versed in the first-aid responses of various kinds. In case of a bleeding nose, you need to prevent the blood from running down the throat and also to cause the bleeding to stop. To achieve this, you should sit down while pinching your nose right below the end of the bone. At the same time, you should lean to the front to prevent the blood from entering your throat. Keep your nose pinched for a while. Check every five minutes if the bleeding is stopped. However, continue at least until four checks in severe cases even if the bleeding has stopped. You should also avoid being hard on your nose and don’t breathe or blow from your nose out of discomfort. Also, avoid moving your head and try your best to rest for a while. In severe cases, such as a fracture, you must go to the doctor and get the treatment. There are also some different factors and things that you should take care of to properly stop the bleeding from the nose. Some of these steps include:
- Pinch tightly with your forefinger and the thumb, not too tightly to hurt the injured area.
- Make sure that you don’t lean back as an attempt to stop bleeding and keeping the blood in.
- You can also use a nasal gel or antiseptic inside your nose to prevent infection.
- Get enough rest afterward
- While most people try to do that out of confusion, it’s common sense to understand that it won’t happen. You can’t stop the flowing blood by leaning back, and it will enter your throat, and you will end up puking which can put further pressure on the injured nose.
Preventive measures for Nosebleeds
You don’t have to have a nosebleed to start thinking about preventing it from happening the next time. As an athlete or a sportsman, you should always be aware of this possible danger that you can face at any point in your game or career. Here are some of the effective preventive measures you can keep in mind to avoid yourself from getting a nosebleed
- Extreme weight lifting or similar exertions can burst your thinner blood vessels resulting in a nosebleed
- Avoid picking and irritating your nose
- Avoid nose blowing
- After the injury, avoid unnecessary drugs like aspirin for a few days
- Use an antiseptic gel
- Always act according to your doctor’s advice
- Practice preventive measures during your training
Achilles tendon injury
What Is an Achilles tendon Injury?
An Achilles tendon injury is a common medical condition experienced by many people involved in sports and athletics. However, people who aren’t involved in sports can also suffer from Achilles tendon injury. Achilles tendon is the largest tendon in the entire human body. It starts from the heel and extends towards the calf area. If you touch the back of your ankle, you will be able to feel it as a flexible extension of tendons stretching from the top of your heel. Injury of this tendon is quite normal, and the condition can be mild or severe. Usually, the common symptoms are a pain, burning a stiffness in the leg with the limitation of mobility. The tearing can be partial or complete.
Causes
Some different things can cause Achilles tendon injury. Some of the most common causes associated with Achilles tendon injury are:
- Pivoting
- Speeding up and slowing down at once
- Dancing
- Baseball
- Basketball
- Tennis
- Soccer
- Athletics and gymnastics
- Running
- Football
- Softball
- Volleyball
The most common situation that leads to this problem is when you lift your foot before you start running. Depending on how fast you want to run, this lift can put serious pressure on the Achilles tendon which can result in an injury and trauma ranging from mild to moderate and severe in certain cases. This situation is most commonly seen during the sprinting as the runner starts the run. Risk factor associated with Achilles tendon injury is age, which puts the people over the age of 30 years under high risk of Achilles tendon injury. Also, males are more prone to getting Achilles tendon injury compared to females. Other causes and risk factors associated with Achilles tendon injury include:
- Having flat feet which causes the stretching of tendons as the arch of the foot touches the ground while taking the steps. The condition is also known as fallen arches.
- Side effects of certain medication and antibiotics can cause Achilles tendon injury in some people and greatly increase the risk.
- Wearing high heels is physiologically very unhealthy and puts the ladies at high risk of developing Achilles tendon injury or a related condition.
- Tightness in the muscles of the legs as well as the tendons due to certain reasons. Tearing can occur if these muscles and tendons are too tight.
Symptoms
There are some different symptoms that people with Achilles tendon injury may experience through the span of the injury. However, it greatly varies from patient to patient and the condition and severity of each case. In less severe cases the patient may experience a sudden discomfort in the ankle and heel area during a walk or run. In most cases, ACL cases include a sudden pain emerging from the ankle along with the loss of control over the proximal muscles. In severe cases, the movement of the foot is severely limited, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling. Other symptoms associated with the condition may include
- A quick and intense pain behind the ankle after receiving a tight stretch.
- Muscles are clenching or cramping in the calf area in certain cases.
- Tenderness in the area of the injury
- A tugging feeling or sensation of loss of strength in the foot.
- Inability to continue kicking, jumping or sprinting.
- Snapping and popping sound
- Inability to move normally without limping.
- Continual, severe discomfort in the lower leg area.
Symptoms are usually made worse when a person with an Achilles tendon injury attempts to move their knee and the ankle joint when traveling upstairs, or attempting to run, jump, or kick.
Secondary symptoms of an Achilles tendon injury wound include tightness, soreness, and stiffness after long periods of not moving, including when waking up after a long sleep.
Achilles tendon injury‘s chief symptom is a pain at the back of the foot above the heel. However, there are several other symptoms associated with the condition. These include:
- pain that seems to come on suddenly
- increasing pain when you lift your foot
- pain when stretching your foot joint
- Muscle spasms at your calf.
- tenderness to the touch at the back of your ankle
- swelling or bruising
You may feel this pain when running or walking.
The pain associated with hip flexor strain is quite specific. You may notice:
- Pulling sensation in the back of the ankle
- Muscle spasms
- Weakness
- Tenderness upon touching the area
- Swelling or inflammation
- A limp while walking
- A visible muscle deformity, in cases of severe tears
Diagnosis
The diagnosis is initialized by the doctor in which primary parameters are observed at first. This includes the patient’s medical history as well as the physical examination. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain, tenderness and other symptoms. In the lying position or knelt position, the doctor may squeeze the calf muscle to see if the tendon is still connected or if it is torn.
The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. If the Achilles tendon is damaged, the movement of the foot and calf become difficult and painful for the patient.
Once the initial examination is performed, and the doubts are reduced, the doctor may follow up with diagnostic procedures. The techniques used in this case are radiographic investigations, ultrasonography and if necessary, the doctor may also use MRI scans to find out the exact location of the damage.
From acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine position, and the movement and flexion of the leg are examined.
Treatment
Mild condition and in some cases moderate injuries can also heal naturally after rest and proper care. In severe cases, more attention is needed. Nonetheless, in either scenario, it’s important to take certain measures to ensure a speedy recovery and healing of the patient from Achilles tendon injury. The treatment can be administered in different ways. Here is the most effective approach for the treatment of this problem.
- Cut down on physical activities as much as possible
- Maintain a regular stretching habit to lengthen your calf muscles under expert supervision.
- Avoid sports or change the sports which don’t involve the injured area.
- Use ice on a regular basis for up to a week.
- Always keep your foot elevated when sitting or lying
- Use aids, such as crutches and braces.
- Use footwear accessories and proper shoes
- Keep up with a proper physical therapy
- To alleviate pain, use over the counter drugs and anti-inflammatory medicines.
- Wear shoes with a heel or use an addon insole.
Apart from these approaches, there are other treatment options available. Some state or the art and advanced treatment options are platelet-rich plasma technique, steroid injections, and ART.
If the non-surgical treatments are not working out for you, you may require surgery. Surgery is a better option than leaving the problem unattended. If the problem is ignored, it can cause a rupture which worsens the symptoms. A surgical procedure is required and administered in which the injured area is exposed by opening the skin, and the torn tendons can then be put into place by the physical administration of suturing and sewing. For the surgery of Achilles tendon injury, you may undergo an open repair surgery. It involves an incision in the heel bone and sewing the torn or ruptured tendon back on its place. Otherwise, you may undergo another method that involves the use of needles for putting the ruptured tendons in the right place. It can also prevent the reversing of the condition which is more common in non-surgical options. The healing process is accelerated with the help of the surgical procedure, and people who require to get back on their feet sooner can do so. Since surgical procedures are more invasive, there are risk factors that are associated with surgical procedures, such as a chance of getting an infection, bleeding, damaging the nerves accidentally during the surgery, clotting of the blood, anesthesia, scarring, and breakdown of the skin. Another unfavorable reason is the high cost associated with the surgery. Enthusiastic and competitive sports people and athletes sometimes go through surgical processes to heal and regain their abilities. In certain cases, delayed diagnosis can turn the Achilles Tendon Injuries into a more severe condition, in case of which surgery may be required on an emergency basis to treat the patient.
Here is a quick to-do list for the treatment:
- Resting as much as possible
- Icing the painting area
- Using compression bandages
- Anti-inflammatory medication
- Exercising, stretching, friendly workouts
- Gradually start physical activities, don’t rush.
- Wearing and using a heel lift.
- Use special shoes or accessories to aid the injured ankle
- Keep up with physical therapies and stretching
- Exercise regularly but only the right ones
- Surgery as a last resort, if no results and symptoms persist after the treatment.
Preventive Measures for Achilles tendon Injury?
Even though Achilles tendon injury is mostly due to accidental causes, you can certainly prevent the condition because it’s mostly due to the patient’s ignorance and mistakes. Here are some of the most effective things you can do to protect yourself from Achilles tendon injury:
- Be careful at the start of your sprinting
- Don’t push up on your toes with too much pressure
- Avoid uphill running
- Learn proper preventive measures in the training
- Reduce training errors with practice
- Wear the right kind of shoes with the right size
- Don’t overdo your workout and avoid getting the overuse syndrome.
Recovery from Achilles tendon injury
In most cases, a rehab therapy results in complete recovery from Achilles tendon injury. Physical therapies along with the RICE treatment can effectively treat the condition and get the patient back on the ground. However, there is a chance of healing process getting reversed if proper measures are not taken and if healing has not completed. Therefore, it’s essential to let your injured muscles recover completely by following the protocol provided by the doctor to eliminate the chances of getting repetitive injuries, chronic conditions, and permanent damage. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area, the type of causes of the Achilles tendon injury and other factors. For your part in effective recovery, you should avoid the normal routine activities according to your doctor’s advice. Depending on the severity, the Achilles tendon injury can take from a few weeks to a couple of months of time to recover. Achilles tendon injury are painful. Therefore, usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. A regular visit to the doctor will ensure that it’s time to go ahead. Here are some other indications for a patient who has recovered from an Achilles tendon injury condition:
- Ability to move the leg and foot easily and freely similar to the other healthy foot
- No pain in walking, running, jumping or jogging
- Regaining the lost strength and overcoming the weakness caused by the injury
Turf Toe
What is a Turf toe?
As the name suggests, a Turf toe is a condition that usually occurs in people involved in certain types of sports that makes use of the feet extensively. The condition is characterized by inflammation and pain in the muscles and tendons related to the area that serve connective purposes, specifically for the big toe. Usually, it’s a minor condition, but it may be very painful at times. It can be a result of overexertion and hyperextension of the big toe. In certain cases, it can result in partial or complete tearing of the ligaments that are associated with the area and which are responsible for the connection of basal and metatarsal phalanx, while in other cases it can be a sprain in these ligaments. People involved in certain sports are more at risk of developing such a condition of a Turf toe, such as wrestlers, dancers, and gymnasts. Footballers and soccer players are also at high risk, as the condition can develop as a result of the big toe being pushed suddenly or repetitively. The condition can develop acutely due to a sudden trauma, or in a continuous manner due to repetitive microtraumas.
Causes of Turf Toe
The condition of a Turf toe is due to the straining of the ligament that connects the two bones in the two and remains responsible for the movement of that down in an up and down motion. These bones are located in behind the toenail and help in providing the leverage during the movement such as running or walking. They also work as the shock absorbents and absorbs the shock on the feet caused by our weight. While we take steps during the walk or while we run, the pressure is transferred from our heel to our toes as we pull our foot up. If the pressure is more or if the angle becomes shorter due to overstretching or an accidental fall, the ligaments there can be severely stretched and pulled. This can result in a sprain, wearing or tearing of these ligaments as the toe is bent beyond its permissible limits.
The most common cause of a Turf toe injury is the turning and the twisting of the toe joint due to displacement. As a result, the toe is pushed out of its normal and natural position, and it can cause muscular and tendon damage. Such unexpected movements are very common in sports that involve a lot of running and the use of legs. These tearing of the muscles can be very painful at times and could be accompanied with other symptoms such as bruising discoloration and the swelling of the area. Although it’s mostly the tendons, ligaments, and muscles that are damaged or injured due to a Turf toe injury, it can also damage other structures, such as the blood vessels and cartilages. There are several risk factors involved, such as the types of sports, etc. however, it can occur in people of all ages.
Some of the other most common causes for a Turf toe injury include:
- Walking on uneven or hard surfaces
- Wearing the wrong sized or kind of shoes
- Rigorous sports activities and feet movements
- Twisting of feet and toe muscles
- Stretching of the toe
- Bending of the toe beyond the normal limits
- Turning suddenly during a play
- Worn out shoes that don’t provide adequate support
- A sudden strain due to kicking
- Running and stopping suddenly
- Continuing sports after mild strains and pain.
- Wrong diagnosis of a previously occurring pain.
- Repeated minor injuries
- Overuse syndrome
- Microtraumas
The onset of a Turf toe injury is usually an acute one, meaning that it is normally caused due to a sudden injury caused during the sports activities. It’s more commonly experienced in players who are involved in sports on artificial and hard surfaces compared to the ground and grace. However, people on the soil and ground can also experience the same condition.
Symptoms of Turf Toe
A-Turf toe injury can result in some different symptoms, and it may vary from person to person depending on the severity of the condition and the type and location of the injury. However, the most common symptoms that indicate that the patient has a Turf toe injury are the following:
- Bruising on the skin
- Discoloration of the injured area
- Tenderness of the injured area
- inability to walk
- Mild to severe pain due to muscular damage
- inability to move the toe joint
- limitation of mobility
- swelling on foot or around the toe
- the stiffness of the injured area
- Quick and intense pain in the toe joint after receiving a tight stretch.
- Muscles clenching or cramping
- A tugging feeling or sensation of loss of strength in the foot.
- Inability to continue kicking, jumping or sprinting.
- Snapping and popping sound
- Inability to move normally without limping.
- Continual, severe discomfort in the foot
However, since toe is prone to some different sports-related injuries, it is easy for a person to mistake it with some other underlying condition which can cause a lot of trouble in the future for the patient. Therefore, it is strongly recommended that once such symptoms start to show up after an injury, the patients should reach out to their doctors as soon as possible for the examination of the condition.
Diagnosis for a Turf Toe
The diagnosis of a turf toe will start when the doctor inquires to the patient about their condition, the symptoms, their professional and personal activities, the type of footwear that they use, the type of their participation in the sports they’re involved in and their history. The diagnosis further includes a physical examination in which the patient is checked for any apparent symptoms of pain and swelling. The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. The doctor may also carefully examine by moving the toe joint in different positions to see if the movement is limited and painful. Numbness is also considered to be an indication. After a physical examination, the doctor may need to carry out a diagnostic test if the doubt persists. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. X-ray test will be able to analyze the bone condition, while the CT scan will help the doctor to locate and study the internal structures to see any possible damage. In certain cases, the diagnostic test may also make use of electromyogram for the determination of possible condition.
By acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely and the severity of it. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine position, and the movement and flexion of the hip and legs are examined. The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain and tenderness.
Treatment for a Turf Toe Condition
Mild conditions of a Turf Toe injury can be treated with proper rest. To speed up the healing and recovery process, further actions can be taken. For this purpose, some different treatments can be administered to alleviate the symptoms and treat the condition of a toe turf injury. The treatment of the injury depends on the grade of the severity, and the approach may vary for grade 1, grade 2 and grade 3 injuries. Here is a complete description of various treatment options used for Toe Turf injuries in order of the severity of the condition.
- Apply the complete P.R.I.C.E protocol on a regular basis.
- Use OTCs and NSAIDs to alleviate the symptoms
- Take proper measure for protecting the toe from further damage
- Use turf toe plate and Morton’s extension
- Limit or completely inhibit mobilization.
- Practices exercises for increasing range of movement
- Do not underestimate grade 1 injuries, as they can gradually worsen
- Take rest as much as possible
- Incorporate anti-inflammatory foods in your diet
- Use ice on the proximal area of injury
- Quit sports for a while
- Change footwear or use add-ons to adjust
- Practice progression exercises
- Use crutches, cane or other aids
- Keep up with your Physical therapy
Special shoes
The shoes that we wear has a lot to do which our feet health. Although wearing the right type of shoe with a complementing sole can reduce the chances of getting a toe turf injury, you can make use of special shoes in case if you already have it. Special medicated shoes can ensure that no further damage is done in the case of a toe turf injury and it also ensures a quicker recovery. Also, avoid walking on the hard surfaces. If you can’t, your medical shoes will help you reduce the pressure on the sensitive and injured toe if you walk on hard surfaces. These shoes are specially designed to take care of the problem of a toe turf injury. There can be an internal padding and special design to wrap around your injured feel and the shape of your feet. Apart from that you can also use similar accessories and add them to your shoes.
Dedicated shoes are specially designed to take care of this problem. They are soft from the inside because of cushioning and wraps around the shape of your foot properly. You can also use the inner cushion or cups for your shoes that come as an accessory.
Preventive measures for a Toe Turf
There are some precautionary measures that you can take to prevent a turf toe injury. The prevention is usually more about common sense and some knowledge, and the patient can understand what is needed to be done with a little knowledge and interaction with the pain. Several preventive measures should be understood and exercised in the fields. The best way to go about it is to practice them during the training until they become your reflexes. The prevention measures can be classified as primary and secondary preventions, and both of them are very important. The risk factors associated with a turf toe injury should also be addressed and taken care of, including the patient’s history of a turf toe injury, the strength of the muscles and the previous injuries. The patients who have experienced previous injuries are two times more susceptible to experience it again upon a heavy blow. Apart from these things, here are the most effective measures you can take to reduce your chances of a turf toe injury:
- Wearing proper sized and shaped shoes
- Avoiding worn out shoes
- Wearing proper sports gears
- Properly using the equipment
- Taking rests and breaks frequently
- Avoid too much repetitive stretching
- Strengthening muscles and making them more flexible
- Communicate with your body and understand what it’s telling you
- Keeping yourself hydrated at all times
- Avoid overexertion and fatigue
- Keep electrolytic balance
- Keep up with vitamins and minerals
- Take healthy nutrition
- Ensure proper intervals and rest time
- Completing the rehabilitation therapy for any previous turf toe injury
- Practice strengthening exercises
- Taping and using a bandage to wrap toe but not too tightly
- Avoid further damage by braces and right shoes.
- Stretching and warm up
- Careful on the uneven and hard surfaces
- Don’t do overexertion and stop when your body tells you to stop.
- Say no to high heels
Recovery for turf toe
A turf toe injury is prone to get reversed in the absence of proper care, and recurring injuries can also take place. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area and other factors. Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. For effective recovery, you should get back to the normal routine activities slowly and gradually according to your doctor’s advice. Once you start using your muscles and bones again, it will complement the complete healing of the injured parts. If the patient were healthy before the injury, the recovery would usually be faster. However, due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the injury can take from 3 weeks to a few months of time to recover.
Tommy John Surgery (UCL Injury)
What is Tommy John surgery?
Tommy John surgery is a relatively new type of surgery that is becoming more and more common for the treatment of sports injuries specifically for UCL injuries. The treatment surgery is named after Tommy John, who was a population baseball player from the Major League since he was the first one to go through this treatment. The surgery is specifically done for the treatment of Ulnar Collateral Ligament injuries usually caused in sports people and athletes. The injury is specific to the elbow area. People who are involved in sports and athletics which makes excessive use of the arm and elbow are more at risk of developing this problem. Ulnar Collateral Ligament is a type of ligament that is found in the inner region of the elbow. The function of this ligament is to ensure that the elbow joint remains stable. If the ligament gets damaged, dislocation of the elbow can take place. It is also important for its connective purposes, as it’s a connective ligament that joins the long bone of the upper arm with the elbow, known as humerus bone with the bones in the forearm, known as the ulna.
The injuries in the Ulnar collateral ligament (UCL) takes place due to chronic micro-traumas in most cases. Repetitive overuse of the elbow and putting stress and pressure on the elbow joint repetitively can cause damage to the internal ligament of the elbow. It’s usually a result of overhead movement of the arm, which is characteristic of certain sports such as cricket, volleyball, baseball, and tennis. People involved in these sports are more at risk of developing Ulnar collateral ligament (UCL) injuries. Given its effective treatment through surgery, the injury is also named after Tommy John, and it’s known as Tommy John injury. Apart from the surgical procedures, the injury of the Ulnar collateral ligament (UCL) can also be treated with the help of physical therapy and rehabilitation process, which can improve the range of movement and alleviate the symptoms to ensure quick and speedy recovery. The condition is characterized by inflammation and pain in the ligament and the proximal area that serve connective purposes on the arm and the elbow. It specifically functions to enjoin the forearm with the elbow. The inner area of the elbow is affected which causes an extending pain towards the forearm. The condition may be mild or severe, and it may be treated easily or require prolonged caring. The painful condition and inflammation are developed due to the overuse and overexertion of the muscles of the arm. This mostly happens in athletes, in cases where the overuse of the arm, too much rotating, gripping and flexing of the wrist can result in inflammation. As a result, the ligaments can be damaged, degenerated and get torn. Nonetheless, the name doesn’t imply that it’s only experienced by sportsmen. In fact, anyone can experience this type of inflammation of ligaments. The initial symptoms of an Ulnar collateral ligament (UCL) injury may vary from person to person and depends on the severity of the condition. However, some common symptoms that occur soon after the onset of the injury are usually tightness and pain in the elbow area. In certain cases, the post-treatment symptoms may reverse the treatment and cause recurring injuries in the absence of proper care from the patient.
Symptoms for UCL
The patients suffering from ulnar collateral ligament (UCL) injuries can experience several symptoms that can indicate the injury and the severity of the injury. The patient can usually experience sharp and sudden pain and symptom of soreness in the elbow region due to the straining. While the symptoms may vary from patient to patient, some of the most commonly observed symptoms of ulnar collateral ligament (UCL) injuries are:
- A pop sound or feeling experienced at the time of the injury
- Internal swelling in the elbow region as well as the extended part of the arm
- Stiffness in the elbow region
- Difficulty in movement
- Limitation of the full range movement of the elbow joint
- Bruising can occur at the injured area
- Discoloration in certain cases
- Tingling sensation from the arm extending towards the hand, causing tingling in the last two fingers
- Weakness in gripping of the arm
- Soreness in the affected region
- Numbness and tingling sensation in the arm
- Swelling in the injured area
- Dislocation of the elbow in certain cases
- Instability of the elbow due to the damaged ligament
- Reduced athletic and sports performance of the patient
- Pain in the affected area of the injury which can spread towards the wrist through the forearm.
- Difficulty and pain in the movement of the elbow
- The difficulty, pain, and weakness in the movement of the wrist
- Tenderness inside of the elbow and extending along the forearm
- Difficulty in doing everyday things, such as pouring coffee, shaking hands, moving the arm, and typing on the keyboard.
Treatment Options for Ulnar collateral ligament (UCL) injuries
Despite the effective Tommy John Surgical option, natural and non-invasive treatments are usually recommended for ulnar collateral ligament (UCL) injuries. The right approach to treat this condition is the treatment of the causes instead of alleviating the symptoms of the condition. It could include a personal treatment plan, healthy diet plan, changes to the lifestyle and exercising regime. Due to the overuse and overexertion, the painful and inflammatory condition can be specifically treated. Ulnar collateral ligament (UCL) injuries are usually experienced by people involved in the different profession, and it’s most commonly found in the people within the age group of 30 to 50 years old. Moreover, it’s experienced by people that practice golf, swimming, painting, tennis, rowing, and baseball. Due to the improper use of the technique, gripping and moving repetitively, and throwing and lifting improperly, ulnar collateral ligament (UCL) can get damaged and injured.
The type of injury and the severity of it will determine the right and effective type of the treatment for ulnar collateral ligament (UCL) injuries. However, some of the common and most effective minimally invasive and non-surgical treatment options available are given below:
Using physical Aids to prevent further damage
Complete P.R.I.C.E. protocol
Acupuncture and massage therapies are known to be effective for UCL injuries
Receive a complete course of physical therapy and rehabilitation program
Changing lifestyle and eating habits
Achieving immobilization with the help of devices
Use corticosteroid injections in severe case
Correcting the Training practices
The corrective action plan is important to ensure that your training habits are not the reasons for your UCL injuries. After consulting a physical therapist, you should give up on the practices that you have been doing wrong all along.
Platelet Rich Plasma (PRP)
This relatively new technique is effective for the treatment of Ulnar collateral ligament (UCL) injuries, and it can provide a quick fix in minimum time. It uses the centrifuge technique to concentrate the platelets from your blood which is injected in the area of injury. So far this innovative technique is effective.
Cortisone injections
Cortisone injections are used to handle the cases which are not cured with the milder treatment options. Although it is an effective way to recover the inflammatory conditions, it is not used as a first choice due to its side effects regarding weakening the tissues and muscles.
Surgery
Tommy John surgery is the most popular and effective option for most UCL injuries. Despite being invasive, it can enable you to get back to your sports and continue playing.
Recovery for the ulnar collateral ligament (UCL) injuries
Usually, the pain is the best indicator to figure out how much more time it will take to recover as you experience a reduction in the degree of pain with time. Recovery time varies greatly from patient to patient depending on the severity of the condition, the strength of the injured area and other factors. It can take anywhere from a week to many months. For effective recovery, you should get back to the normal routine activities slowly and gradually according to your doctor’s advice. Once you start using your muscles and bones again, it will complement the complete healing of the injured parts. If the patient were healthy before the injury, the recovery would usually be faster. However, due to so many factors, it is not possible to precisely tell the time frame. Depending on the severity, the injury can take up to 6 months of time to recover.
Posterior cruciate ligament Injury
Introduction
PCL or Posterior cruciate ligament injury is one of the most common injuries of the knee, commonly experienced by the sportsmen and athletes. The condition can be very painful, and the patient could need knee surgery to get it back to normal. However, each case differs and it depends on the severity of the condition.
What is Posterior Cruciate ligament?
The knee joint is a meeting point of three important bones, the tibia, patella, and the femur. Due to the natural knee cap placement, the joint usually remains protected. Four ligaments are also attached to the bones and the joint, which can be classified as cruciate ligaments and collateral ligaments. The cruciate ligaments are present on the inside and intercept each other. The upper intercepting ligament is termed as anterior while the one below is called the posterior cruciate ligament. The Posterior cruciate ligament (PCL) protects the femur and tibia and keeps them stable. Even though the Posterior cruciate ligament (PCL) is greater in strength and stability as compared to the Anterior cruciate ligament (ACL), the Posterior cruciate ligament (PCL) can get injured and even torn in a similar fashion as Anterior cruciate ligament injuries and tear.
Posterior cruciate ligament (PCL) injury
Posterior cruciate ligament (PCL) injury and a sprain is a result of injuries to the meniscus, knee structure, ligaments and articular cartilage that is present in the area. These injuries can be graded and classified into three main types, depending on the severity of the injury and type of injury. There are different Types of Posterior cruciate ligament (PCL) injury similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three types are:
Type 1: This is characterized by less than moderate pain, while the patient retains the ability to feel and move the injured area.
Type 2: This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
Type 3: This is characterized by severe pain, while the patient loses the ability to feel and move the injured area.
Type 4: This is characterized by severe pain, while the patient loses the ability to feel and move the injured area. In this condition, other proximal ligaments and structures also get damaged.
Causes of Posterior cruciate ligament (PCL) injury
The most common cause of Posterior cruciate ligament (PCL) injury is an accidental injury. Other causes include severe hit, falling on the knee directly, stopping too quickly during a run, and quickly moving in different directions. Women as found to be more prone to Posterior cruciate ligament (PCL) injury due to the tenderness of muscles and ligaments, while men may also experience tearing and spraining.
Posterior cruciate ligament (PCL) injury is more common in people who are involved in cycling, running, athletics, football, soccer, and hockey. The most common reason is the sudden change in the training practices and the exercise regime of the players, or accidental injuries caused during the running.
If an injury causes a sudden weakness and disability, you should see a doctor as soon as possible. The most common cause in sports for this injury is a hard hit, heavy blow or contact sports. As a result, the wearing and tearing can take place in the femur and patella. There are several other causes and risk factors associated with the condition of Posterior cruciate ligament (PCL) injury. The injury can be a result of the wrong kind and size of the shoes which may put pressure on the muscles up along the legs. Other factors are also important such as the intensity of the hit. Overtraining and intense training all also among the most common causes of this condition.
Other causes include:
- Falling on the knee when it is bent
- Striking of knee against a hard surface
- Running several steps
- Suddenly stopping while running
- Legs stretching
- Leg displacement or foot displacement while running.
- Wrong posture and legs movement
- Sudden jerking
- Heavy hit
- Hard blows
Signs and symptoms of the Posterior cruciate ligament (PCL) injury
The onset of the condition can be gradual over time, or it can be acute due to a sudden injury. Depending on the severity, the signs and symptoms can vary. In less severe cases the patient may experience a sudden discomfort in the knee during a walk or run. Diffuse peripatellar pain is experienced in this condition around the kneecap. In most cases, it’s difficult for the patient to identify the exact location of the pain. The patient may feel and experience a grinding feeling with the movement of the knee. Prominent sound and friction occurring due to knee joint movement are also experienced. The patient may also feel a clicking feeling or sound occurring due to movement of the knee. A feeling and a sound of popping in the knee joint upon movement may also occur. In such cases, the injury includes a pop sound from the knee along with the loss of control over the knee muscle. In severe cases, the movement of the knee joint is severely limited, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling. The patient can experience discomfort while walking, bending knees and while sitting. The everyday activities such as walking up or down the stairs can also become a challenging task. Depending on the type of Posterior cruciate ligament (PCL) injury, the signs and symptoms can vary. In severe cases, the movement of the knee joint is severely limited, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling.
Diagnosis for Posterior cruciate ligament (PCL) injury
As we have previously discussed, the diagnosis for the Posterior cruciate ligament (PCL) injury is not always very simple and sometimes require a compound approach. Therefore, a differential diagnosis is commonly carried out for Posterior cruciate ligament (PCL) injury. The diagnosis of Posterior cruciate ligament (PCL) injury is complicated and difficult, which is the reason why it can be easily mistaken as another syndrome, such as, Osgood–Schlatter disease. Prepatellar bursitis, Sinding-Larsen, and Johansson syndrome, plica syndrome and patellar tendinitis. There isn’t any single best method for the diagnosis of the Posterior cruciate ligament (PCL) injury, as the muscle damaged and the conditions can vary among different patients greatly, and many other diseases, problems, and health conditions can result in a similar kind of a pain in the knee. Therefore, a differential diagnosis is administered to eliminate the possibilities of other conditions.
The diagnosis is initialized with a careful examination of the patient’s history as well as the physical examination. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case.
Once the initial examination is performed, and the doubts are reduced, the doctor may follow up with diagnostic procedures. The techniques used in this case are radiographic investigations, X-Ray Tests, the differential diagnosis, and sonographic evaluations. If necessary, the doctor may also use MRI scans to find out the exact location of the damage.
From acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine or elevated position, and the movement and flexion of the knee and legs are examined.
The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain, tenderness of the femur and patella area. The diagnosis also includes the identification of the grading and category for the condition.
Treatment for the Posterior cruciate ligament (PCL) injury
Non-surgical procedures are reported to be successful in most cases of PCL injuries. Surgery is a viable option. However, natural and non-invasive treatments are usually recommended for Posterior cruciate ligament (PCL) injury. Posterior cruciate ligament (PCL) injury is usually experienced by people involved in the different profession and its most commonly found in the people within the age group of 30 to 50 years old. It could include a personal treatment plan, healthy diet plan, changes to the lifestyle and exercising regime. Due to the overuse and overexertion, the painful and inflammatory condition can be specifically treated. The treatment of PCL injuries and PCL tears depend on the severity and condition of the injury. However, various treatment options are advised for all grades of PCL tears. For instance, RICE rule is an initial treatment response for all grades of PCL sprains. Rest must be ensured for the injured area as well as the whole body. Joint immobilization is also important for which aids and braces can be used. To reduce the swelling ice gives effective results. Compression bandages are also used by the patients. The doctor will prescribe you to keep your common and injured area elevated to increase the blood circulation and boosting recovery. Certain anti-inflammatory OTCs and NSAIDs are also prescribed by the doctor, such as ibuprofen and aspirin to relieve pain and other symptoms. After administration of this initial treatment, a closer examination will suggest the right kind of treatment. In case it is a grade one or grade two PCL injury, the knee may get splinted and you will be subjected to a rehabilitation program. It will include straightening of the muscles that are surrounding the knee joint to improve the position and remove the splint. The rehab will also ensure that you do not get a secondary injury.
PRP Technique
The innovative PRP technique can be effectively used for the treatment of Posterior cruciate ligament (PCL) injury. It is a non-surgery procedure that stimulates the healing by injection of concentrated platelet-rich plasma into the affected area. This therapy is used for grade 1 and grade 2 PCL injuries.
If it is a Grade three PCL sprain, the condition will be much more severe, and the treatment criteria will be different. These cases usually involve the complete PCL tears where the PCL is pulled out or torn from the bones. Sometimes this tearing also pulls away a piece of bone with it. The condition is very painful and requires a proper initial treatment protocol. Afterward, surgery is performed to reattach the torn PCL back to its place either by sewing or which the help of a screw. For this purpose, a part of the ligament is taken from the proximal area of the patient’s injured leg, which is known as the donor site. This donor tissue is referred to as an autograft or allograft depending on the area from where it is taken. This surgical procedure usually adopts the technique of arthroscopy and a camera lens. Once the surgery is completed, and the reconstruction is achieved, long and steady braces are used to hold the knee and the leg at a certain position until it is healed to avoid further tearing.
Surgical treatment for PCL Tears
In certain severe cases, surgery may be required to fix the problem. It becomes critical when the patient requires immediate recovery, when the injury persists, or when the injury keeps bending and displacing the knee. The surgery may also be required if multiple ligaments are injured. In the surgical procedure, the damaged ligament is removed and replaced by another tissue known as a graft, which allows it to heal and recover. The graft may be taken from a donor area which is usually another area of the knee. However, rehabilitation is still required after the surgery. The surgery is minimally invasive and reconstructs the damaged ligament.
Surgery is usually prescribed to the Posterior cruciate ligament (PCL) patients, as it can effectively recover the patients bringing them back to the normalized knee condition. However, if the patient isn’t involved in heavy activities, such as jumping, running, too much manual work, or sports, the alternative treatment options can be administered.
The surgical treatment is initiated after a delay of around one month. This is usually done to monitor the healing speed of the patient and let the swelling and bleeding reduce. This also gives an idea of the persistence of the injury. Physiotherapies are essentially involved in the post-operative rehabilitation therapy. The recovery highly depends on the consistent care and physiotherapeutic treatment, without which the recovery may be delayed or reversed. It’s important to note that the surgical treatment also requires few to several months of rehabilitation therapy and the sportsmen can return to the playgrounds after a year. The process starts with light exercises and later on the focus is gradually shifted towards enabling the full-range movement of the knee joint. Flexing and bending your muscles too much should be avoided, and the gradual increase in the exercising routine should be practiced. The rehabilitation therapy also uses aids like crutches and braces to improve the protection level and prevent pressure, jerking and stress.
Preventive Measures for Posterior cruciate ligament (PCL) injury
It’s important to stick to proper training and exercising methods to avoid getting a Posterior cruciate ligament (PCL) injury due to a training accident. Sportsmen and athletes should also be mindful of the possibility of a knee injury and should be aware of measures to prevent the knee from severely damaging in case of an accident. Should be aware of measures to prevent the knee from severely damaging in case of an accident. Another effective way of preventing Posterior cruciate ligament (PCL) injury is to strengthen the core muscles by exercising. Some exercises such as hamstring can help increase the strength and endurance of leg muscles. Stronger legs can also help to reduce the pressure on the knee due to falling. Athletes and sportsmen must also practice techniques of jumping, cutting, pivoting, proper knee positioning and landing to prevent injury from sudden falling.
Skier’s Thumb
What is Skier’s Thumb?
Skier’s Thumb injuries can be defined as the injuries that are caused to the soft tissues and the ligament of the thumb that results in palpation, pain and other symptoms. The proximal ligaments are damaged due to trauma or repetitive micro-traumas in typical cases. The condition is also referred to as the Gamekeeper’s thumb or an ulnar collateral ligament (UCL) tear. Depending on the severity of the condition, the ulnar collateral ligament (UCL) can get damaged, sprained or even torn in severe cases. In the majority of the cases, the ulnar collateral ligament (UCL) injury can result in an avulsion. Ulnar collateral ligament (UCL) injury or Skier’s thumb injury is caused to the soft tissues known as ligaments. Soft tissues can be defined as the tissues that usually serve the purpose of the surrounding, supporting and connecting other tissues, organs, bones and structures inside our body. This group of soft tissues may include the nerves, tendons, muscles, fascia, and tendons. There may be other structures involved in this group as well, such as blood vessels, fibrous tissues, synovial membranes and the fats. Wearing and tearing of soft tissues can be relatively more comfortable and may cause severe problems. Ulnar collateral ligament (UCL) has the function of connecting the bones of the thumb to one another, and it also aids in the movement of the bone joints in the thumb. The name of this injury was tossed as gamekeeper’s thumb in 1955 when the first classified case was recorded. Apart from sudden and acute trauma, it can be caused due to repetitive movement and twisting of the thumb. Since this injury is quite common in people involved in Skiing, it was later termed as the Skier’s thumb injury. Many people involved in other sports are also at risk of developing this condition as a result of an injury. The treatment choice for this is based on the severity of the situation and the damage caused by the injury. The Ulnar collateral ligament (UCL) injury can take place in the form of a sprain, partial tearing, or in certain severe cases complete tearing of ligament and its avulsion from the bone. In such cases, a surgical procedure may be required to fix the problem and recover the patient. If surgery is avoided in cases of severe damages, the stability of the ligament with the thumb can be compromised, and the recovery can be slowed down. As a result, it can result in a permanent deterioration of the grasping function of the thumb. Physical therapy and a process rehabilitative process are essential to ensure that the treatment gives best results. In most cases, people can continue with their sports activities after proper treatment.
Skier’s Thumb Causes
A blow, hard hit or a trauma to the ligaments, and tendons can cause Skier’s Thumb injuries. The most common cause is bending of the thumb backward with too much force which can damage or completely tear the ligament. The condition is characterized by pain, swelling, and other similar symptoms. Skier’s Thumb injuries can result from some different causes, including anything that can potentially damage the ligament. It usually occurs in pain and can be accompanied by some different symptoms. Some of the most common causes of Skier’s Thumb injuries in the field of sports could be:
- Falling
- Bending the thumb backward
- Bruising
- Heavy blow
- Bursitis
- Twisting of muscles
- Sudden trauma
- Tendonitis
- Sprains
- Strains
- Sudden jerking
- Heavy hit
Signs and Symptoms for Skier’s Thumb injuries
Skier’s Thumb injuries can cause acute symptoms. Pain is the most important symptom of Skier’s Thumb injuries which can be aggravated by the movement. The pain can either be chronic or develop gradually over a long term, or it can be due to a sudden injury or blow in most cases. Difficulty or complete loss of movement ability is also experienced by the people suffering from Skier’s Thumb injuries. Occasionally the patient may also experience swelling, redness, and warming of the injured area. The symptoms you should generally look for are the following:
- Feeling pain and stiffness
- Swelling of the injured thumb
- Increased pain occurring due to compression
- Difficulty or inability of moving thumb in some instances
- Blue or black discoloration of the injured thumb
- Losing the ability to grip and grasp
- Increased pain due to movement
- Pain spreading towards the wrist
- Sharp and intense pain in the start
- Gradual dulling of the pain
- Bruising and rashes
- Sharp and stinging pain while using the thumb
- Tenderness
- Discomfort
- Redness
- Weakness
- Instability
- The inability of function due to severe tearing
The degree of Skier’s Thumb injuries
There are different grades for Skier’s Thumb injuries such as strains and sprains, similar to other injuries, depending on the severity of the injury, condition and the symptoms occurring in the patient. The three grades are:
Degree 1
This is characterized by less than moderate pain, while the patient retains the ability to feel and move the injured area.
Degree 2
This is characterized by moderate pain, while the patient partially retains the ability to feel and move the injured area.
Degree 3
This is characterized by severe pain, while the patient loses the ability to feel and move the injured area.
Diagnosis for Skier’s Thumb injuries
The physician will first determine whether or not the patient has other limb-threatening injuries and then evaluate the thumb in more detail. After that, an examination of the physical condition and the patient’s medical history will be conducted. The specialist will ensure if the patient is suffering from damage to other injuries that can threaten the function of the limb. A close evaluation of the thumb is carried out. The doctor may move the muscles, and check for pain, swelling, palpations, tenderness and other physical symptoms. The condition is also tested by a squeeze procedure, in which the injured part of the patient is squeezed to check for pain, tenderness and other symptoms.
The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. If the Thumb is damaged, the movement of the thumb joint becomes difficult and painful for the patient. Along with the history check the doctor may go through an interview with the patient and inquire about several medical facts related to the patient based on the following subjects:
- The exact time of the injury
- Reason and cause of the injury
- If the thumb was stressed or bent more than normal limits
- The time it took after the injury to show symptoms of swelling and pain
- The exact position of the thumb and hand during an injury
The questions based on the medical history may include:
- Previous incidences of similar traumas
- Natural hand orientation of the patient
- Any underlying conditions
- Previous events of fracturing the hand bones
- Any allergies to different treatments
- Any history of the surgical procedure of the hand
Once the initial examination is performed, and the doubts are reduced, the doctor may follow up with diagnostic procedures. The techniques used in this case are X-ray tests, and if necessary, the doctor may also use MRI scans to find out the exact location of the damage.
By acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely. This phase includes thorough examination and assessment of every individual and unique case. The physical examination may include:
Laxity testing: the tip of the thumb is moved sidewards while holding it from the base to see the angle of movement which is compared to the angle of the excellent thumb’s movement.
Checking for fractures and tenderness.
Assessment of the three central nerves of the hand to see if they’re correctly functioning
Treatment for Skier’s Thumb injuries
There are several ways to treat the Soft Skier’s Thumb injuries. The treatment may vary depending on the severity of the injury and the type of the underlying cause of Skier’s Thumb injuries. Most cases of skier’s thumb injuries are treated with non-surgical procedures. The treatment can be classified as the first aid initial response treatment and the long-term treatment. Initial response differs for severe cases. For mild to moderate injuries, the long-term treatment plan also differs from severe cases, as it is more focused on the rehabilitation therapy instead can surgery and operative procedures.
After the proper diagnosis of the condition, a careful evaluation of the seriousness of the issue is conducted by the doctor for skier’s thumb injury. The immediate response includes icing, rest and painkillers. Various drugs are available in the market that can be used for pain relief and reduce the inflammatory conditions. Typically, the NSAIDs are used at the initial stages of the treatment. Splints are used to immobilize and stabilize the thumb as a movement may worsen the condition. These are usually put on for a couple of months to ensure that the healing is assisted with the help of this aid. There are a variety of different designs for splints available in the market. You may require a particular design and type depending on your condition. The doctor will analyze the condition of your thumb injury and decide the right design for you accordingly. Physical therapy especially associated with the thumb is practiced under the supervision of a specialist. You may require this therapy during the time of immobilization period. This will include some different exercises to improve and enable full range movement and prevent stiffness during the time of immobilization. It is also essential to strengthen the ligaments to avoid secondary injuries. Physical therapy along with a proper immobilization tool will be able to effectively cure around 90 percent of total cases of skier’s thumb. Once treated. You must only get back to using your thumb in your everyday activities gradually. The gradual progression is essential to prevent any further damages and to reverse the entire treatment. If the condition of skier’s thumb persists after all the useful treatment options, you may opt for surgery to avoid the risk of chronic instability. You can also couple up your approach with energizing and vitalizing foods that can improve the healing ability of the body. If the pain is disturbing you, you can try putting rice in the area of injury around the splint, but make sure that you do not take it off.
Non-surgical procedures usually treat Skier’s Thumb injuries unless the injury is extremely severe. Nonetheless, the treatment method depends on the severity, degree and the type of injury. In case if the surgery is needed, you will be sent to the relevant orthopedic surgeon and a reexamination will take place. If you’re a fit candidate for the surgery, the surgeon will aim at repairing your damaged or torn ligament by suture anchor. In simple words, this treatment requires the torn ligament to be sewed back to the right place which helps it heal faster and speeds up the recovery. It also removes the chances of dislocation of the ligament which can impact the functionality and the movement of the thumb. A lightweight cast is used after the surgery to keep the thumb firmly in the right place to let the ligament heal properly. This cast needs to be worn for a while until your doctor advises you to take it off. In case there is a secondary fracture along with Skier’s Thumb injury, then a fracture stabilization is also carried out in the same procedure.
Preventive Measures for Skier’s Thumb injuries
There are some precautionary measures that you can take to prevent Skier’s Thumb injuries. Stretching of the muscles is an excellent way to build resilience against Skier’s Thumb injuries. In repeated injuries, the stretching can be done by softly allowing the muscles and ligaments to move and function in the proper way they’re meant to function. That should be achieved through physical therapy. The prevention is usually more about common sense and some knowledge, and the patient can understand what is needed to be done with a little knowledge and interaction with the pain.
- Wearing proper sports gears
- Properly using the equipment
- Taking rests and breaks frequently
- Learn preventive measures for accidents during play
- Gradually increasing the intensity of the workout
- Always hold your weights in a confident and right way
- Strengthening ligaments and making them more flexible
- Communicate with your body and understand what it’s telling you
- Ensure proper intervals and rest time
- Keeping yourself hydrated at all times
- Avoid overexertion and fatigue
- Keep electrolytic balance
- Keep up with vitamins and minerals
- Take healthy nutrition
Meniscus Tear Injury
A Meniscus Tear Injury is a common medical condition experienced mostly by people involved in sports characterized by rupturing and tearing or a single or multiple fibrocartilage strips known as menisci. In most cases of torn cartilage, the cause remains to be the damage or tearing of the meniscus. The most common tearing occurs at the top of tibiae. Specific activities such as squatting, walking, running and other activities of sports can cause this tearing. Regarding sports injuries, acute traumas and overexertion remain to be a prevalent cause. It could occur due to the twisting and bending of the knee and cause degenerative conditions.
Meniscus Tear Injury can result in swelling and pain in the knee joint. It can either occur as an acute condition or as a chronic condition developed by repetitive microtraumas. Some other symptoms can also be expressed varying from patient to patient, which includes motion locking, clicking, pop sound, and catching. The pain can increase as the load is put on the knee. In severe cases, Meniscus Tear can also be accompanied with the damage to other proximal ligaments such as ACL and MCL ligaments, which can result in a common condition known as an unhappy triad. The meniscus cartilage serves to protect and cover the knee joint which is the largest joint in our body, against the stress that is caused to it due to bending, running, climbing and walking. Hyper-flexing of the knee also results in tearing of the meniscus. Some different treatment methods may be used for the recovery of a torn meniscus. Physical therapy in case of Meniscus Tear Injury is very effective regarding strengthening the muscles, recovering the injury and stabilizing the knee joint. In severe cases or when other treatment options do not show significant results, then a surgical procedure may be required to treat the problem.
What causes a meniscus to tear?
The most common cause of a Meniscus Tear Injury is the turning and the wrong training habits, forcefully twisting and turning, suddenly stopping while running, imbalance of the muscles, and sudden displacement. It can also be caused due to the grinding of the femur against the tibia. As a result, the ligaments can get seriously damaged due to friction and rubbing, and knee can be pushed out of its normal and natural position, and it can cause muscular, ligament and tendon damage. Such unexpected movements are very common in sports that involve a lot of running and the use of legs. These tearing of the muscles can be very painful at times and could be accompanied with other symptoms such as bruising and the swelling of the area. Although it’s mostly the fibrocartilage that is damaged or injured due to Meniscus Tear Injury, it can also damage other structures, such as the blood vessels, ligaments, tendons, the knee by displacing it, and nerves. There are several risk factors involved, such as the types of sports, etc. however, it can occur in people of all ages.
Some of the other most common causes for Meniscus Tear Injury include:
- Lifting heavy weights
- Walking on uneven or hard surfaces
- Wearing the wrong sized or kind of shoes
- Squatting
- Kneeling
- Rigorous sports activities and feet movements
- Twisting of feet, leg and knee muscles
- Turning suddenly during a play
- A sudden strain due to kicking
- Running and stopping suddenly
- Continuing sports after mild strains and pain.
- Microtraumas
- Wrong diagnosis of a previously occurring pain.
- Repeated minor injuries
- Overuse of the muscles
- Long training hours
- Sitting in the lotus position for long hours
- Prolonged running on an uneven surface
- Uphill and downhill running
- Climbing and descending stairs again and again
- Not stretching and warming up before workout and running
- Hiking for long hours
- The weakness of cartilage and muscles
- Obesity and overweight
- Older age
- The reduced supply of blood
Signs and symptoms
The symptoms and signs of Meniscus Tear Injury can vary from person to person depending on the severity of the condition. In less severe cases the patient may experience a sudden discomfort in the knee during a walk or run, or sometimes no symptoms at all. The pain may go once the patient rests for a short while. For some people, the pain is not experienced suddenly and may build up gradually with time. In most cases, Meniscus Tear Injury cases include a stinging sensation in the knee along with the loss of control over the knee muscle, which may destabilize the knee. In severe cases, the movement of the knee joint is severely limited due to the pain, and gradually physical signs start showing up, which may include severe pain, muscular tenderness, and swelling. Some of the other most common symptoms can include:
- Thickening of the tissue in the proximal region
- Burning sensation
- Increased pain with the passage of time
- Pain due to the striking of the foot on the ground
- Persisting pain in the Meniscus
- Pain in the tibia upon compression
- Weakness and feeling of the knee giving away
- Increased pain due to running and walking
- Popping sound or feeling
- Tearing and disability of movement
- Tenderness of muscles
- Pain in adduction movement and closing the legs
- Popping or snapping feeling
- Locking of the knee
Diagnosis
As the initial response, the doctor will first of all look at the patient’s condition. In later phases, the doctor may demand a medical record of the patient and ask to get certain tests done. The doctor may do a few things, such as moving the muscles and checking for pain, swelling, palpations, tenderness and other physical symptoms. The doctor may also test the condition by using the traditional squeeze procedure, in which the injured part of the patient is squeezed to check for pain, tenderness and other symptoms. In the lying position or knelt position, the doctor may squeeze the proximal region to see if the function is disabled.
The medical history also has a lot to tell about the condition, and it’s essential for an effective treatment of the patient in this case. If the Meniscus is damaged or torn, the movement of the foot and calf become difficult and painful for the patient.
Once the initial examination is performed, and the doubts are reduced, the doctor may follow up with diagnostic procedures. The techniques used in this case are radiographic investigations, ultrasonography and if necessary, the doctor may also use MRI scans to find out the exact location of the damage. Depending on the individual case and the severity of the condition, the doctor may conduct an MRI (magnetic resonance imaging), an ultrasound test or an X-Ray Test. For the examination of tendons, muscles, and ligaments, MRI will provide sufficient evidence for possible damage. An X-ray test will be able to analyze the bone condition.
By acquired results, a careful evaluation is performed by the doctor to ensure the condition of the patient precisely. This phase includes thorough examination and assessment of every individual and unique case. The patient is laid in a supine position, and the movement and flexion of the leg are examined.
Arthroscopy is also another widely used technique for the diagnosis of Meniscus Tear Injury. Previously it was used more than it’s used today for diagnosis due to advancement and further.
non-invasive methods for diagnosis. However, this option is still used for the surgical procedure in several severe cases of Meniscus Tear Injury. In this diagnosis, a small tube which has a scope is inserted inside of the knee structure to analyze and see the precise location of the damage and the condition. Once it is analyzed, the arthroscopic surgery may be used to treat the damage caused due to Meniscus Tear Injury. In this diagnosis, a small tube which has a scope is inserted inside of the knee structure to analyze and see the precise location of the damage and the condition.
Treatment Options for Meniscus Tear Injury
Despite the effective surgical option of arthroscopy, natural and non-invasive treatments are usually recommended for Meniscus Tear Injury. Meniscus Tear Injury is usually experienced by people involved in the different profession and its most commonly found in the people within the age group of 30 to 60 years old and above. The treatment of the causes is important for the cure of meniscus tear injuries. It could include a treatment plan, healthy diet plan, changes to the lifestyle and exercising regime. The most important factor is the physical therapy and rehabilitation that comes into play. In severe cases, the long-term treatment may also include a surgical fixture. The problem can occur due to the overuse and overexertion. Moreover, it’s experienced by people that practice sports that involve feet and legs such as soccer, running, jogging, football, basketball, and others. Due to the improper use of the technique, twisting and moving repetitively, and running and lifting improperly, Meniscus can get damaged and injured.
The treatment choice depends on the grade and severity of the condition of Meniscus Tear Injury. However, some of the common and most effective minimally invasive and non-surgical treatment options available are given below:
The initial treatment takes the approach of protection, rest, ice, compression, and elevation.
After the first aid, you must make sure that you rest your knee as much as possible. The traditional PRICE protocol is administered for all grades of meniscus tear injuries. You can also use crutches and braces to ensure immobilization and improved healing. You must also avoid lifting any kinds of weight. At the hospital or home, you will be required to keep your leg elevated whenever you’re sitting or lying down. The swelling can be reduced by using ice on the injured area regularly for a few days. Each session of icing should be done for 30 minutes, and four sessions are recommended throughout the day. Compression bandages can also be used to alleviate the inflammatory condition. The medication will be initially prescribed traditionally. These medicines would include non-steroid anti-inflammatory drugs and pain relievers. You should also avoid walking as it requires you to put full weight on the legs. If it is painful, you may use crutches or a cane. Physical therapy will follow the traditional initial treatment in the long run. This will ensure that you do not experience stiffness due to lack of mobility. In case of severe injuries and complete tearing, you will be required to have surgery along with the post-operative rehab therapy.
For grade 3 injuries, an arthroscopic surgical procedure is mostly in practice. It is reported to show effective results in most grade 3 cases. You will be given pre-operation instructions that should be followed. It will also require a deeper examination with more tests. Arthroscopic surgery is a widely used technique for the treatment of Meniscus Tear Injury. In this surgery, a small tube which has a scope is inserted inside of the knee structure to analyze and see the precise location of the damage and the condition. Once the condition is fully analyzed, the arthroscopic surgery may be done to treat the damage caused due to Meniscus Tear Injury. This can help ensure speedy recovery and faster healing of the cartilage. Another surgical procedure known as microfracture surgery can also stimulate the healing and growth of new cartilage. In this treatment, new holes are drilled in the bone. However, it is not workable for meniscus cartilages, and it doesn’t produce stronger cartilage.
The surgery may take into consideration certain previously underlying health conditions, such as an infection, fever, cold, fever, wounds and other issues. A small incision will be made on the knee to let the arthroscope enter the damaged area. The instruments will be passed through the arthroscope to cut out the damaged part or repair a complete tear by screw or sewing procedure. The surgery may take 1 to 2 hours to complete, and you will be able to go home the same day. Post-operative care will be crucial, and a rehab follows up will be required. It may take a few months to recover from rehab in severe cases. Meanwhile, you can gradually go about your daily activities while using the crutches and canes. For some patients, there may be an underlying risk associated with the surgery. This may vary from person to person, and you should have a detailed discussion with your doctor regarding the possible risk factors.
Summary of Sports Injuries
Sportsmen and athletes can be susceptible to different injuries. The most effective way to keep yourself safe as a sportsman is a prevention through proper training and natural treatment methods. Almost all people involved in sports experience sports-related injuries at some point in their life. The most common types of sports injuries among all of these are Shin splints, Ankle Sprains, Tennis Elbow, Groin Pull, Knee injuries, Hamstring Strain, and ACL tearing. RICE treatment therapy (Rest, Icing, Compression and Elevation) is an effective therapeutic method for the treatment of most injuries. Severe cases may require surgery or steroid injectable, but these treatment methods should be the last resorts. Proper diagnosis of the treatment is important to ensure the effectiveness of the treatment. Some risk factors are associated with sports injuries, and the most common factors are the strength of your muscles and bones and the age group. Learning about sports injuries can not only protect you from injuries but also keep you healthy while protecting your entire career as a sportsperson.
References
Ready, G. (2018). Hip Flexor Pain: Causes, Treatment, and Prevention.
Health, V. (2018). Hip Flexor Strain – The Complete Injury Guide.
William Morrison, M. (2018). Hip flexor strain: Symptoms, causes, and treatment.
Hip Flexor Strain: Causes, Symptoms, and Treatment. (2018).
Hip Flexor Strain. Causes, Symptoms and Treatment. (2018).
Sports injury. (2018)
Sport Injury Treatments by MedicineNet.com. (2018).
Chris, D. (2018). Soft Tissue Injuries Types, Causes, Symptoms, Treatment | Healthhype.com.
Benjamin Wedro, F. (2018). Rotator Cuff Injury Symptoms, Tests, Treatment, Healing Time & Pictures.
Benjamin Wedro, F. (2018). Rotator Cuff Injury Symptoms, Tests, Treatment, Healing Time & Pictures.
Tennis Elbow vs. Golfer’s Elbow: The Causes, Symptoms and Treatments | North Jersey Orthopaedic and Sports Medicine Institute. (2018).
Tennis Elbow vs. Golfer’s Elbow: Causes, Symptoms & Treatments. (2018).
Rotator cuff injury – Symptoms and causes. (2018).
Common Shoulder Injuries – OrthoInfo – AAOS. (n.d.).
Haddad, A. (n.d.). 3 Common Shoulder Sports Injuries.
Non-Surgical Treatments for Tennis and Golfer’s Elbow Pain. (n.d.).
Wheeler, T. (2017) Hamstring Strain. Web MD
Payne, J. (2018, January 03). Hamstring Injuries | Causes and Treatment.
Hamstring Muscle Injuries – OrthoInfo – AAOS. (2015)
Sciatica Animated Video. (1999).
Hochschuler, S. H. (2016). Sciatica Surgery.
Hochschuler, S. H. (2016). Physical Therapy and Exercise for Sciatica.
Jr, W. C. (2018). Sciatica Treatment, Causes, Symptoms & Exercises.
Hochschuler, S. H. (2016). What You Need to Know About Sciatica.
What Are Shin Splints? Web MD.
Complete Guide to Shin Splints (2017).
Carlson, C. (2018, May 25). 4 Exercises to Prevent Shin Splints.
Shin Splints. (2018). Sports Injury Clinic
Groin Strain: Symptoms, Treatments, and Recovery Time. (2018) Health Line
Groin Pull. (2018). Web MD
Groin Strain. (2018) Sports Injury Cinic
Groin strain. Physiopedia
Groin Strain: Symptoms, Treatments, and Recovery Time. (2018)
Stöppler, M. C. (2018). Muscle Cramps Causes, Treatment, Prevention, Symptoms & Types.
Muscle cramp: Causes, Symptoms and Diagnosis. (2018). HealthLine
Nordqvist, C. (2017, December 14). Fractures: Types, causes, symptoms, and treatment.
Bursitis. (2017, August 12).
Hip Bursitis Symptoms, Treatment, Recovery Time & Exercises Patient Comments: Hip Bursitis – Treatment – Viewers Share Their Medical Experiences.
Stress Fractures. (2018). Sports injury clinic.
Bursitis. (2018). FootSmart
Cole, G. W. (2018). Athlete’s Foot Treatment, Causes & Symptoms.
Concussion (Traumatic Brain Injury). Web MD
Brain Injury Pictures: Concussion Causes, X-Rays, and Treatments. (2018).
Facts About Concussion and Brain Injury. (2017, November 17).
Concussion. (2017, July 29).
ACL injury. (2018, March 13).
Course Directions
-
When you are finished reading the course & are ready to take the quiz, click the link underneath the Quizzes Section that says “Survey Questions” to complete the survey.
-
After you complete the survey, follow the steps to take the Quiz.
-
After you complete the quiz with a passing score of 70% or higher, your certificate will be available to view & save for your records.
-
You have 3 attempts to obtain a passing score on the quiz.
Helpful Tip: In case you need to double check an answer while taking the quiz, leave the Lesson Material OPEN by right clicking the “Survey Questions” link to open the Quiz in a new tab.